
How has the new Shockwave C2+ catheter changed the treatment of calcified coronary lesions at Herzzentrum Lahr/Baden (Lahr, Germany)? Kambis Mashayekhi and his team—Emmanouil Chourdakis, Sven Moos and Myron Zaczkiewicz—detail their intravascular lithotripsy (IVL) journey, including a case study involving a diffuse calcified left main bifurcation.
Intervention in calcified coronary lesions remains a challenging field. Proper lesion preparation is associated with better lumen gain, stent expansion, and arterial compliance, as well as easier stent delivery, with lower rates of stent thrombosis and periprocedural complications.1
IVL is a well-established and safe plaque modification technique for the treatment of severely calcified coronary stenosis, regardless of plaque morphology (superficial or deep, concentric or eccentric).2,3 The Shockwave device is a single-use semi-compliant balloon catheter with a very short learning curve and fast preparation compared to atherectomy devices, without wire bias or device entrapment.
At the 2023 Cardiovascular Research Technologies (CRT) conference (25–28 February, Washington DC, USA),4 new research demonstrated that IVL is histologically superior in cracking coronary calcium compared with conventional balloon angioplasty treatment. However, we should not rely on evidence of fracture to confirm IVL effectiveness, as optical coherence tomography (OCT) has the potential to fail to identify the presence of calcium fractures and underestimate the depth of fracture compared to microcompted tomography (micro-CT).4
Our intracoronary journey with IVL began five years ago with de novo short calcified lesions. Over time, we have increasingly been confronted with severely calcified longer stenosis, including the off-label use of IVL for in-stent failure.5,6
One issue that has been raised in the past has been pulse delivery, which, at 80 pulses, limited the device to shorter segments. The new Shockwave C2+ catheter is now suitable for treating longer calcified lesions with an increased number of pulses from 80 to 120 (10 pulses per cycle). The additional 40 pulses allow the preparation of longer calcified lesions with different distribution patterns within the same patient. Thus, not only can superficial and concentric lesions be treated with a single catheter, but also nodular and eccentric lesions—which usually require more extensive modification with a higher pulse rate.
Calcified lesions that cannot be crossed with the Shockwave catheter may require prior plaque modification with atherectomy, colloquially referred to as “rotashock” therapy. This modifies superficial calcification, and facilitates balloon delivery for further modification of deep calcification by IVL, particularly in larger lumina.7
IVL has been adopted in our routine clinical practice for the treatment of calcified left main disease as it provides safe plaque modification with less perceived haemodynamic instability, less carina shift, and protection of the side branches by the guidewire during pulse delivery.8,9 IVL 3.5 or 4mm catheters provide good balloon apposition to the vessel wall, resulting in a greater effect of therapy with more lumen gain, tackling both superficial and deep calcification.8,9
Intracoronary imaging with intravascular ultrasound (IVUS) or OCT is key to understanding plaque morphology, proper IVL balloon sizing, management, planning and optimisation of percutaneous coronary intervention (PCI).10
The new Shockwave C2+ catheter can be used in all conventional guiding catheters (5, 6 or 7Fr) in combination with extra supportive guidewires, balloon anchoring techniques and “mother-in-child” catheters to significantly improve support for balloon delivery.
Case study
This case study demonstrates the possibilities of the new Shockwave C2+ balloon, detailing the treatement of a 67-year-old male patient with IVL for a diffuse calcified left main bifurcation.
A transradial approach with a 7Fr sheath from the right radial artery was chosen. A 7Fr XB 3.5 guide catheter (Cordis) was engaged into the left main ostium, placing a Sion blue extra supportive guide wire (Asahi Intecc) into the peripheral left anterior descending (LAD) artery and a Runthrough (Terumo) guidewire in the left circumflex (LCX) artery.
 For IVUS imaging, the HD 60MHz imaging catheter (Boston Scientific) was used to assess the calcium and lesion characteristics. (Figure 1) Due to significant calcium burden of the left main bifurcation with deep calcification, as well as a calcified nodule on the medial LCX, we decided to use a 3.5mm Sockwave C2+ IVL catheter, sized 1:1 based on IVUS in order to achieve optimal plaque preparation.
For IVUS imaging, the HD 60MHz imaging catheter (Boston Scientific) was used to assess the calcium and lesion characteristics. (Figure 1) Due to significant calcium burden of the left main bifurcation with deep calcification, as well as a calcified nodule on the medial LCX, we decided to use a 3.5mm Sockwave C2+ IVL catheter, sized 1:1 based on IVUS in order to achieve optimal plaque preparation.
Pulses were delivered at low pressure (4atm) and the pulse management strategy involved 20 pulses at the ostial proximal/ostial LAD, 40 pulses at the ostial LAD/left coronary artery (LCA), 30 pulses at the ostial LCX/LCA and 30 pulses at the medial LCX.
 Afterwards, IVL outcomes were assessed by imaging (Figure 2), and a 1:1 non-compliant balloon used to check the need for additional IVL or other plaque modification techniques. The non-compliant balloon was fully expanded with no need for further plaque modification after IVL. Based on the left main morphology (Medina 1-1-1), we decided to go for a two-stent strategy. IVUS-guided inverted culotte stenting was performed to treat this unprotected distal left main stem bifurcation disease.
Afterwards, IVL outcomes were assessed by imaging (Figure 2), and a 1:1 non-compliant balloon used to check the need for additional IVL or other plaque modification techniques. The non-compliant balloon was fully expanded with no need for further plaque modification after IVL. Based on the left main morphology (Medina 1-1-1), we decided to go for a two-stent strategy. IVUS-guided inverted culotte stenting was performed to treat this unprotected distal left main stem bifurcation disease.
The first stent was implanted (Onyx TruStar, Medtronic 3.5x33mm) from LCX to LCA, and the second from LAD to LCA (Onyx TruStar 3.5x33mm), followed by kissing balloon dilatation with a 3.75mm non-compliant balloon in each branch. A final post optimisation technique was performed with a 5mm non-compliant balloon at the carina level. A third stent was placed into the medial LAD (Onyx TruStar 3x26mm), followed by 3.5mm n
on-compliant balloon dilatation, finished with the implantation of a fourth stent at the ostial left main (Onyx TruStar 5x12mm). A proper stent apposition and stent expansion was achieved without signs of major dissection on IVUS (Figure 3).
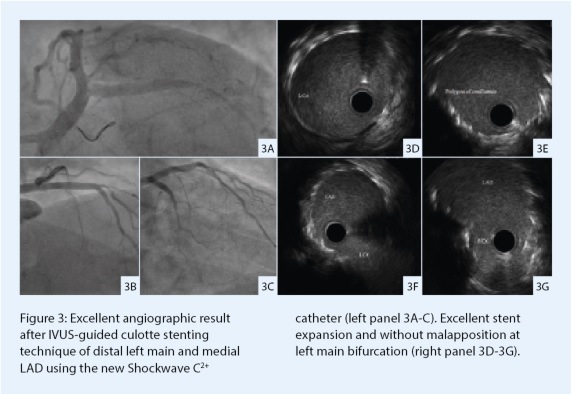 An excellent primary angiographic result with Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow and sufficient stent expansion was achieved. The patient remained haemodynamically stable during the procedure and was discharged the next day.
An excellent primary angiographic result with Thrombolysis in Myocardial Infarction (TIMI) grade 3 flow and sufficient stent expansion was achieved. The patient remained haemodynamically stable during the procedure and was discharged the next day.
IVL treatment with the new Shockwave C2+ catheter offers several advantages in the treatment of heavily calcified coronary lesions, demonstrated in our left main intervention. The ability to deliver more pulses contributes to a more effective and efficient procedure. Overall, IVL therapy has a low rate of major flow-limiting dissections and subsequently a lower rate of haemodynamic instability, providing a safe technique for plaque modification in bifurcation lesions, with the capability to continuously protect the side branch, making the Shockwave C2+ IVL catheter one of the most important protagonists in calcified complex coronary lesions.
References
1. Généreux P, Madhavan MV, Mintz GS, et al. Ischemic outcomes after coronary intervention of calcified vessels in acute coronary syndromes. Pooled analysis from the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) and ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) TRIALS. J Am Coll Cardiol. 2014 May 13;63(18):1845-54.
2. Brinton TJ, Ali ZA, Hill JM, et al. Feasibility of Shockwave Coronary Intravascular Lithotripsy for the Treatment of Calcified Coronary Stenoses. Circulation. 2019 Feb 5;139(6):834-836.
3. Kereiakes DJ, Virmani R, Hokama JY et al. Principles of intravascular lithotripsy for calcific plaque modification. J Am Coll Cardiol Interv. 2021;14:1275–92.
4. Kawai K, Sato Y, Hakoma JY. Histology, OCT, and micro in Atherosclerotic Cadaver Arteries treated with Intravascular Lithotripsy. Cardiovascular Research Technologies. 2023 Feb 25–28 February; Washington DC, USA.
5. Tovar Forero MN, Sardella G, Salvi N, et al. Coronary lithotripsy for the treatment of underexpanded stents: the international & multicentre CRUNCH registry. EuroIntervention. 2022 Sep 20;18(7):574-581. doi: 10.4244/EIJ-D-21-00545.
6. Dwivedi P, Dhulipala V, Kumar KR, et al. Efficacy and Safety of an Upfront RotaTripsy Strategy in the Treatment of De Novo and In-Stent Restenosis Cases. J Invasive Cardiol. 2023 Feb;35(2):E70-E74
7. Cosgrove CS, Wilson SJ, Bogle R, et al. Intravascular lithotripsy for lesion preparation in patients with calcific distal left main disease. EuroIntervention. 2020 May 20;16(1):76-79
8. Salazar CH, Gonzalo N, Aksoy A, et al. Feasibility, Safety, and Efficacy of Intravascular Lithotripsy in Severely Calcified Left Main Coronary Stenosis. JACC Cardiovasc Interv. 2020 Jul 27;13(14):1727-1729.
9. Mintz GS. Intravascular imaging of coronary calcification and its clinical implications. JACC Cardiovasc Imaging. 2015 Apr;8(4):461-471.
10. Hill JM, Kereiakes DJ, Shlofmitz RA, et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease. J Am Coll Cardiol. 2020;76:2635–46.











