By Bernhard Meier
Two studies—RESPECT (Randomized evaluation of recurrent stroke comparing PFO closure to establish current standard of care treatment) and the PC Trial—failed to show that percutaneous closure of patent foramen ovale (PFO) significantly reduces the risk of recurrent stroke. Bernhard Meier reviews the future role of PFO closure in the light of these studies.
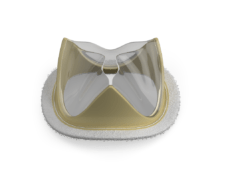
Percutaneous closure of atrial septal defects was first reported in 19751 and preceded coronary angioplasty by at least three years. Following an initial report of PFO closure to prevent recurrent stroke2, the procedure started to draw the attention of those working in adult cardiology. Since then, an estimated 1,000,000 percutaneous PFO closures have occurred worldwide. About 25% of the global population have PFO and, therefore, are potential candidates for percutaneous closure. The closure technique is straightforward and has matured to be the most safe and simple procedure in interventional cardiology to date. However, the proof that PFO closure prevents recurrent strokes or mortality better than conventional medical treatment can only be derived from meta-analyses and therefore is still pending according to statistical purists.
The available facts
At the moment, the established facts are: the PFO remains patent in at least 25% of young adults and this percentage decreases with age. Two, not mutually exclusive, explanations for this decrease are spontaneous PFO closure occurring throughout life and PFO-selective mortality.
Clots in the venous system are virtually non-existent before adult life but then become increasingly frequent. If they migrate to the pulmonary circulation, this goes clinically unnoticed in most cases as they only block an insignificant pulmonary artery until they are lysed by local plasminogen activator. However, if they can get to the systemic circulation through a PFO, they cause relevant cerebral, myocardial, or other sensitive tissue ischaemia.
Aggravating features of a PFO (size of the gap, atrial septal aneurysm, or Eustachian valve) increase the risk of paradoxical embolism.
The risk of paradoxical embolism increases with age (more venous thrombotic material), although this is compensated for at least in part by higher left atrial pressure. Paradoxical embolism is by no means limited to otherwise healthy individuals. Hence, it is illogical to think about it only in the case of so-called cryptogenic stroke.
The PFO can be closed in an outpatient procedure under local anaesthesia with no recovery period or subsequent restrictions. Procedural and long-term complications are exceedingly rare.
The risk of a PFO having become clinically manifest to cause a recurrent event under conventional treatment is 1% per year and not 3%–10% as previously assumed. All randomised trials have been underpowered to a various degree because of that misconception.
Studies
The PC trial (414 patients) was started in 2001 and was published recently—at least seven years later than initially planned3. It showed an 80% reduction in recurrent stroke (five in the control group, one in the treatment group), but this was not statistically significant. The comparable and larger RESPECT trial (980 patients) was endpoint-driven (stopped at 25 strokes)4. By “intention to treat”, it missed statistical significance (16 in the control group and nine in the treatment group).
However, it reached the endpoint of significantly reducing recurrent stroke by the “as treated” analysis (16 and five strokes, respectively; p = 0.007). Joining the “intention to treat” results of the two trials, significance in favour of treatment was reached (21 strokes in the control group and 10 in the closure group).
A third trial, the CLOSURE I trial5, used an inferior device that has been abandoned since and the difference in favour of PFO closure was much smaller and far from being significant.
It can be assumed that adding a couple more years to the protocol-based follow-up duration of the trials will render them individually significant. Comparing data of two comparable randomly allocated (albeit not randomised) patient groups with closure or medical treatment and a follow-up of about 10 years showed a significant mortality and stroke benefit of closure.6
Three randomised trials are ongoing, but I am not sure they should. Even short of clean randomised single-study proof that PFO closure is superior to medical treatment, there is no doubt that it is at least competitive and probably superior.
While one can argue that closure should not be presented as the recommended treatment, it should at least be mentioned as an option. The patient then has the choice between an innocuous short procedure (call it a mechanical vaccination) or life-long blood thinners with their inherent risk growing with age. As a bonus fewer other embolic events such as myocardial infarction or limb ischaemia, and in some patients, improvement in migraine, exertional dyspnoea, sleep apnoea, or platypnoea orthodeoxia come for free. The minimal risk of developing atrial fibrillation or free wall erosion because of the device is imputed in the overall benefit.
References
1. King et al. Surgery 1974; 75:383–88
2. Bridges et al. Circulation 1992; 86: 1902–08
3. Meier et al. N Engl J Med 2013; 368: 1083–91
4. Carroll et al. N Engl J Med 2013; 368: 1092-100
5. Furlan et al. N Engl J Med. 2012; 366: 991–99
6. Wahl et al. Circulation 2012; 125: 803–12
Bernhard Meier, Cardiology, Bern University Hospital, Bern, Switzerland