Peter Haworth (Portsmouth Hospitals University NHS Trust, Portsmouth, UK) documents how computer-derived fractional flow reserve (FFRct) has been instrumental in optimising care in the cath lab at his institution, even despite the challenges created by the COVID-19 pandemic.
Peter Haworth (Portsmouth Hospitals University NHS Trust, Portsmouth, UK) documents how computer-derived fractional flow reserve (FFRct) has been instrumental in optimising care in the cath lab at his institution, even despite the challenges created by the COVID-19 pandemic.
Since it was mandated by NHS England last year, many cardiologists will be aware of, or are actively using, FFRct to help diagnose coronary artery disease (CAD). It is technology we have been using within our service at Portsmouth for some time now, having initially adopted it in 2018 to support our computed tomography (CT)-first approach.
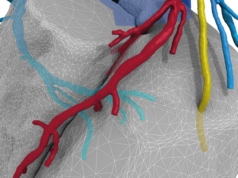
For those unfamiliar, FFRct is a non-invasive, artificial intelligence (AI)-enabled diagnostic test that takes data from a coronary CT to create a 3D, digital model of a patient’s coronary arteries. The technology uses sophisticated algorithms to calculate the severity with which arterial stenoses may be impacting blood flow.
Clinicians are given FFRct values alongside the model so they can quickly understand if CAD is present, where blockages may be and whether invasive intervention is required.
For many cases, the insights provided by FFRct give us confidence that patients can be treated with medication alone. But it is also a tool I use increasingly to support procedural planning in the cath lab, and it has been invaluable in helping to minimise patient contact whilst prioritising the most urgent cases during the pandemic.
Triaging patients
The more we know about a patient’s CAD severity, the better we are able to plan the best course of action.
A CT-first approach often gives us what we need, but FFRct really comes into its own for those scans where disease or the nature of a blockage is unclear. The technology gives us both anatomical and physiological insights which have been instrumental in significantly reducing the number of patients we send to the cath lab at Portsmouth.
This has been especially useful during the COVID-19 pandemic, where we have had limited bed spaces and restrictions on the number of people we can bring into the department. In these circumstances, it is essential we bring in the right patients who will get the most benefit from further investigation or revascularisation. It has also allowed us to be as efficient as possible with the care we are delivering, reducing the time our patients spend in the hospital.
In the cath lab
Once patients are scheduled for the cath lab, I have increasingly been using FFRct to aid interventional procedures. In fact, since I am able to view the entire coronary tree non-invasively with the FFRct model, I am often able to plan out a complete strategy for the patient before they are on the table.
Using the data and modelling available, I can assess the type of revascularisation required—for example, is more complicated bifurcation stenting needed or can we opt for a simpler intervention?

I also use the technology to plan the angles of the procedure—it shows us where to position the C-arm to get the best angiographic images of the vessels as we are working. This has meant less time searching for the best angles and potentially less radiation exposure and time on the table for the patient.
And when it comes to explaining our plans to patients, having a well-rounded strategy before the procedure and a visual 3D digital model on hand during conversations is particularly useful in helping them feel fully informed about their condition and comfortable with the next steps.
Despite the disruption of the pandemic, our cath lab is now as busy as it has ever been. But due to the clarity gained through FFRct the patients we see arrive in the cath lab have anatomical, plaque composition and physiological information which allows us to optimise their treatment. Our need for diagnostic angiograms has dramatically reduced and as we continue to grow increasingly confident in using technologies such as these, it is likely to fall even further. As a result, we have freed up time and space in the cath lab for other essential services such as electrophysiology and pacing. FFRct has also been instrumental in identifying patients who could be considered for clinical trials.
FFRct has been integral to streamlining the diagnostic process and improving patient experience. For me, it speaks to the value of embracing new technologies to optimise delivery of care and continue to improve patient experience.
Peter Haworth reports no relevant financial disclosures.