By David Smith
Individuals with acute coronary syndrome (ACS) represent the largest group of patients undergoing percutaneous coronary intervention in the UK today. In the last few years, patients with ACS, including patients with ST segment elevation myocardial infarction (STEMI), non-ST segment elevation myocardial infarction (NSTEMI) and unstable angina, have overtaken the stable angina population in volume.
The optimal management of patients with ACS includes assessing the risk of a future cardiac ischaemic event following onset, as well as the risk of a bleeding complication from intensive medical therapy or an invasive cardiac procedure (Hillis and Lange, 2009). Currently, the standard treatment for many ACS patients is revascularisation therapy accompanied by the long-term administration of dual antiplatelet therapy, up to one year, to prevent the recurrence of ischaemic coronary events. Interventional cardiologists treating ACS patients, therefore, face a challenge with this standard of care – the notable risk of a bleeding complication.
In general, patients with stable coronary artery disease (CAD) will initially receive optimal pharmacological therapy, and, if this fails to control symptoms, they will undergo planned elective angioplasty. They will receive dual antiplatelet therapy, after which a stent is usually implanted as part of their angioplasty procedure. Following percutaneous coronary intervention, stable patients will receive antiplatelet therapy per standard-of-care to manage their coronary artery disease.
Patients with ACS, in contrast, present acutely and often have co-morbid problems that present an increased risk of bleeding for their dual antiplatelet therapy maintenance. These patients also receive more aggressive in-patient therapy. As soon as ACS patients are admitted to the hospital, they receive immediate antiplatelet and antithrombotic therapy. Regardless of the patient’s level of risk, recommendations for treatment include antianginal therapy, dual antiplatelet therapy and statins, unless contraindicated (Hillis and Lange, 2009).
As a result of the agents they receive while in hospital, the intensity of their therapy increases bleeding risk. This combined with co-morbid medical problems means that they are at a relatively greater risk for bleeding in the short, medium and long term, which can lead to severe complications.
Endothelial cell capture and shorter-term dual antiplatelet therapy
Recent advances in coronary stent technology have been important for clinicians who hope to tailor their treatment to the challenges of each unique patient. For instance, a coronary stent that permits a shorter duration of antiplatelet therapy has the potential to address the challenge of bleeding risk in patients with ACS.
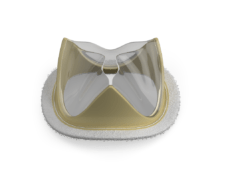
The Genous Stent (OrbusNeich) is one such stent that combines a cobalt chromium scaffold with an anti-hCD34 antibody coating to capture circulating endothelial progenitor cells (EPCs). These EPCs form a functional endothelial layer over and between the stent struts. The unique design of the Genous Stent has been shown in previous clinical trials to enable the safe reduction of dual antiplatelet therapy duration to as little as 12 days (Piscione et al. 2011).
In the treatment of ACS, Genous has the potential to provide a better balance between the efficacy needed to prevent further coronary events, but at the same time providing some degree of protection from bleeding events when they occur. If a bleeding event does occur, it can be just as catastrophic and deleterious to the patient as a recurrent coronary event.
GATEWAY Registry
The newly-initiated GATEWAY Registry is a multicentre, observational registry in the UK designed to reflect real-world practice in patients with ACS.
Much of today’s clinical data are derived from populations that exclude patients who are at a high risk of bleeding. Specifically, ACS patients who are considered to be at significant risk of bleeding are an important subset of patients treated with percutaneous coronary intervention that have not been well-observed.
GATEWAY is recruiting 280 patients at eight sites in the UK for whom clinicians have concerns over their risk of bleeding and who have been treated with a Genous Stent. The study protocol recommends that, instead of receiving 12 months of dual antiplatelet therapy, these patients undergo three months or less following stent implantation.
The primary endpoint of GATEWAY is the occurrence of net adverse clinical events at 30 days and one year follow-up, with net adverse clinical events defined as a composite of major post-procedural bleeding and major adverse cardiac events consisting of death, myocardial re-infarction and target vessel revascularisation for ischaemia or stroke.
We hope to demonstrate that Genous offers an enhanced balance in this high-risk patient population between protection against further coronary ischaemic events and also a reduction of bleeding events in the year post-follow up. From an anti-ischaemic perspective, Genous offers better protection from further ischaemic events than bare metal stents currently do. At the same time, a shorter-term duration of dual antiplatelet therapy compared to drug-eluting stents is very attractive.
Previous clinical trial data for the Genous Stent leads us to believe that we will see efficacy comparable to drug-eluting stents with regard to restenosis and freedom from coronary events, but without the bleeding risk and cost of a year’s worth of dual antiplatelet therapy, which is not desirable in this particular high-risk population.
David Smith, Regional Cardiac Centre at Morriston Hospital, Swansea, UK, is the principal investigator of the GATEWAY Registry trial.