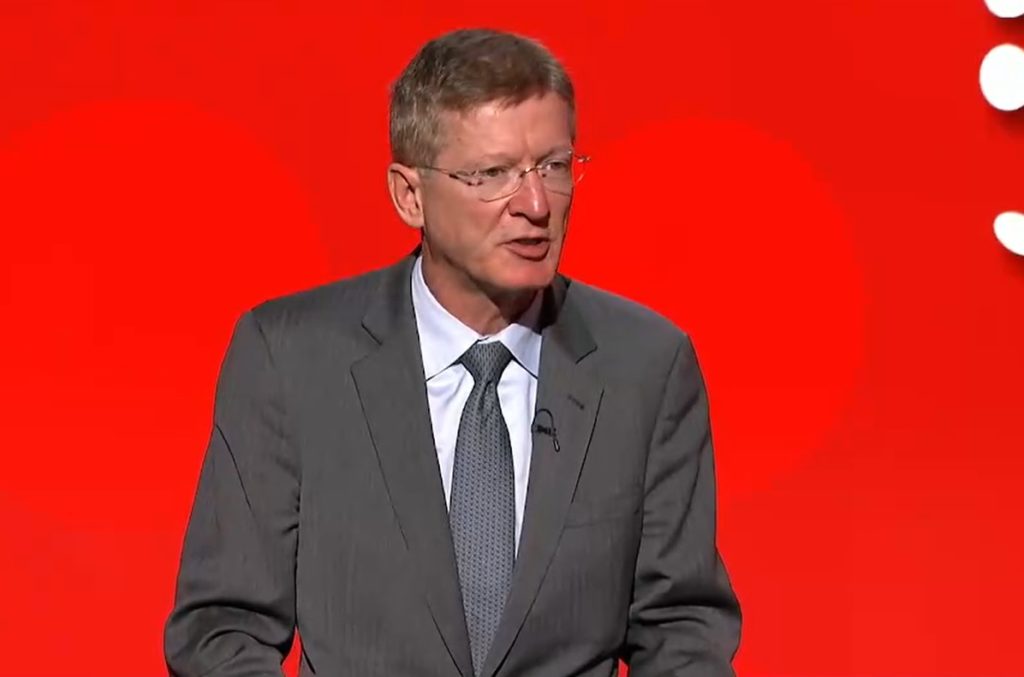
Use of a novel, venous external support device (VEST, Vascular Graft Solutions) may lead to increased longevity and durability of saphenous vein grafting during coronary artery bypass graft (CABG) surgery, according to investigators in the VEST trial, results of which were present by John Puskas (Icahn School of Medicine at Mount Sinai, New York, USA) at the American Heart Association’s Scientific Sessions 2021 (AHA 2021; 13–15 November; virtual).
The VEST trial, which was conducted by the National Heart, Lung and Blood Institute Cardiothoracic Surgical Trials Network in collaboration with the Mount Sinai health network, investigated the safety efficacy of VEST, a small device comprising a braid of 42 cobalt-chromium wires that is placed over a pencil-sized vein graft. The external support is designed to prevent veins from stretching under higher pressure, thereby leading to better survival of vein grafts and improved patient outcomes.
The initial phase of the research, which is the first US Food and Drug Administration (FDA)-approved trial to test the efficacy of this support device, will prompt further long-term studies that may lead to FDA approval, according to investigators.
Proliferative intimal hyperplasia of saphenous vein grafts (SVGs) after CABG predisposes to the later development of graft atherosclerosis and occlusion, resulting in adverse clinical outcomes, Puskas told AHA attendees. External support of SVGs, therefore, has the potential to prevent SVG dilation, Puskas noted in his presentation
“Vein grafts have a limited durability—about half of them will be closed 10 years after coronary bypass surgery. We need to find a solution to improve outcomes of surgery and prevent patients from having complications and repeated procedures,” said Puskas, the trial’s principal investigator.
To study VEST’s efficacy, researchers conducted a randomised patient trial in 17 cardiovascular surgery centres in Canada and the USA between January 2018 and February 2019. They enrolled 224 patients scheduled to undergo CABG with two or more saphenous vein grafts. Patients were their own controls: for each patient, one vein graft was supported with VEST and the other vein graft or grafts had no external support. Investigators used the thickness of the inner cell layer lining the vein graft as the trial’s primary endpoint. To assess this, researchers placed a catheter inside the vein graft and conducted an intravascular ultrasound (IVUS) 12 months after surgery.
In all, 203 of the 224 patients returned for the one-year follow-up angiogram and IVUS. However, 90 of them did not have not have IVUS completed for both vein grafts, due to narrowed grafts or other technical reasons including catheter issues; for these patients, researchers replaced missing information with substituted values from estimates based on data already collected from other patients in the trial.
Data from these 203 patients showed that VEST did not significantly reduce intimal hyperplasia in vein grafts after CABG, compared to non-VEST implanted vein grafts. But when researchers did the same type of analysis on the subset of 113 patients who did complete ultrasounds on both VEST and non-VEST grafts, the VEST grafts had statistically significantly lower amounts of hyperplasia compared to non-VEST grafts.
“These findings are encouraging despite the fact that the p-value of the primary analysis did not quite reach statistical significance. It may be important to note that among patients with complete intravascular ultrasound data the VEST was associated with statistically reduced intimal hyperplasia,” Puskas commented.
The investigators plan to continue follow-up of these patients for five years after surgery.













