Analysis of health status and quality of life data from the TRILUMINATE Pivotal trial, presented at TCT 2023 (23–26 October, San Francisco, USA) indicates that patients undergoing transcatheter edge-to-edge-repair (TEER) for severe tricuspid regurgitation provides “substantial” benefits for symptoms, functional status and quality of life compared to medical therapy, investigators have reported.
Suzanne Arnold (Saint Luke‘s Mid America Heart Institute/UMKC Kansas City, Missouri, USA) presented the data, which investigated the use of the TriClip (Abbott) device, during a late-breaking clinical trial session at the TCT meeting.
Primary results of the trial were presented at the 2023 American College of Cardiology (ACC) annual scientific session (4–6 March, New Orleans, USA), where it was reported that the transcatheter device was effective in reducing TR and led to improvements in quality of life at one year. However, the results did not show any significant difference in survival or heart failure hospitalisation between patients treated with the interventional approach or with medical therapy, the study’s control arm, with the the superiority of the device in meeting its composite primary endpoint primarily driven by improvements in quality of life for patients.
Investigators performed an in-depth analysis of the health status outcomes to describe the timing, magnitude, and consistency of the health status benefits and to estimate the biologic correlates of health status after the procedure and the clinical relevance of the health status benefit.
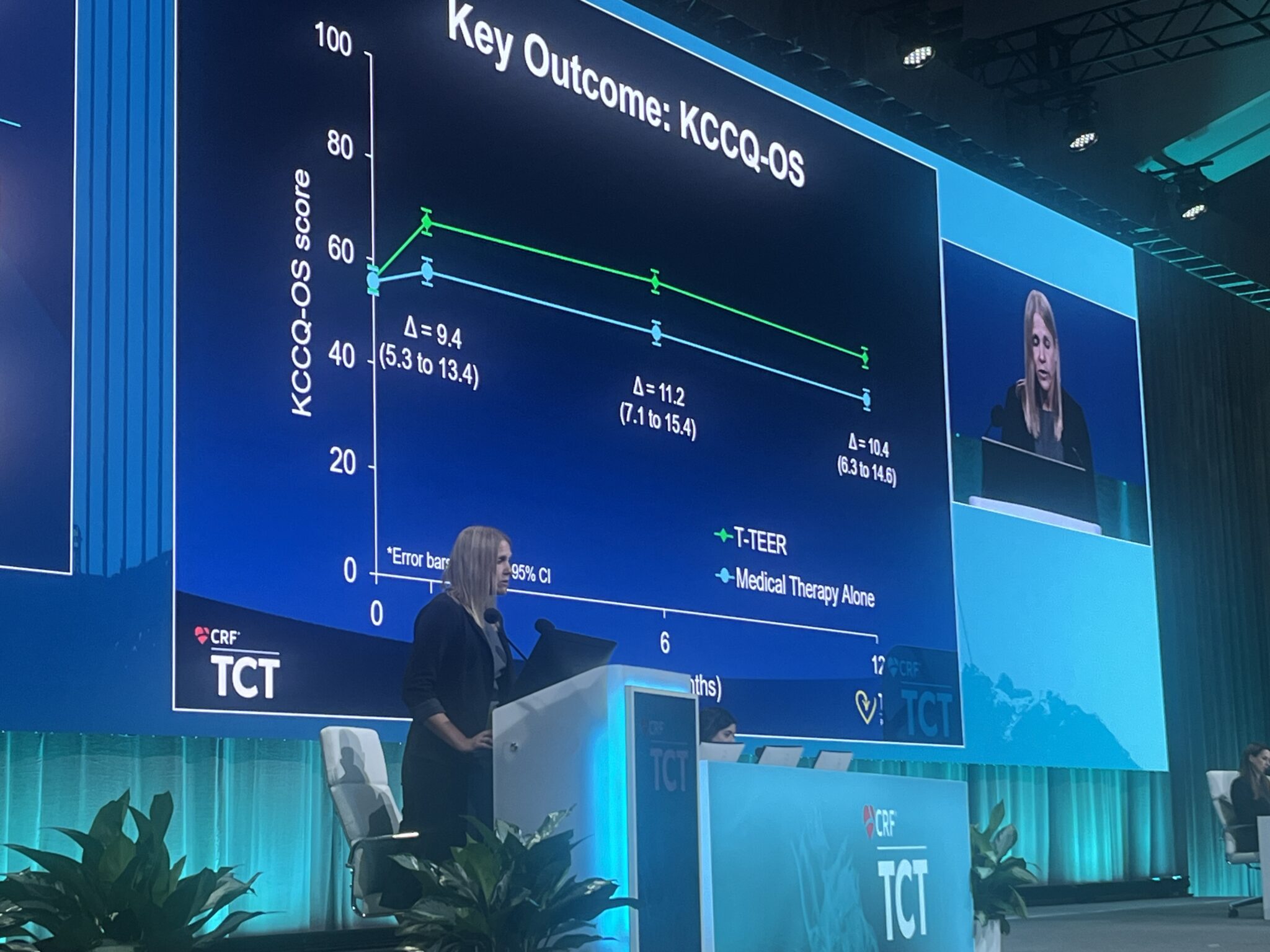
The trial randomised patients with severe TR to TEER (n=175) or medical therapy alone (n=175). Health status was assessed at baseline as well as at one, six, and 12 months with the Kansas City Cardiomyopathy Questionnaire (KCCQ) and at baseline, one and 12 months with the Medical Outcomes Study Short-Form 36 (SF-36) Health Survey.
The primary health status endpoint was the KCCQ overall summary score (KCCQ-OS; range 0-100; higher=better) which was compared between treatment groups using mixed effects linear regression. Alive and well at one year was defined as KCCQ-OS greater than or equal to 60 and no decline from baseline greater than 10 points.
Compared with medical therapy alone, TEER resulted in significantly greater improvement in the KCCQ-OS at one month (mean between-group difference 9.4 points, 95% CI 5.3-13.4) with a small additional improvement at one year (mean between-group difference 10.4 points, 95% CI 6.3-14.6), Arnold reported. Improvements in quality of life were greater among those with the most severe symptoms. Interaction analyses demonstrated that the benefit of T-TEER diminished as baseline KCCQ-OS increased.
TEER patients were also more likely to be alive and well at one year compared to those who received medical therapy alone (74.8% vs. 45.9%, p<0.001) with a number needed to treat of 3.5 to derive benefit.
“As with any medical procedure, the impact on a patient’s quality of life is an important factor in assessing its success,” said Arnold. “Compared with medical therapy alone, TEER resulted in substantially better health status at one month that was sustained through one year. These findings support the use of TEER with the transcatheter tricuspid valve repair system for improvement in the symptoms, functional limitations, and quality of life in patients with severe TR.”