An analysis of structural valve deterioration in the PARTNER 2A trial has found that the third generation Sapien 3 transcatheter heart valve (Edwards Lifesciences) has similar durability to surgical valves, with the second generation Sapien XT (also Edwards Lifesciences) demonstrating lower midterm durability than surgery. Philipe Pibarot (Quebec Heart and Lung Institute, Quebec, Canada) presented the data on behalf of the PARTNER 2A investigators at PCR London Valves 2019 (17–19 November, London, UK).
Other findings were that five year rates of structural valve deterioration (SVD)-related haemodynamic valve deterioration (HVD) and bioprosthetic valve failure (BVF) were higher following transcatheter aortic valve implantation (TAVI) with the second generation Sapien XT than surgery, but four year rates of SVD-related HVD and BVF were similar in Sapien 3 intermediate risk patients and in those undergoing surgical valve replacement. Most reinterventions were related to endocarditis in surgery patients, to SVD in Sapien XT, and to paravalvular aortic regurgitation (AR) in Sapien 3 patients; 30-day mortality related to reinterventions was lower in TAVI than surgery.
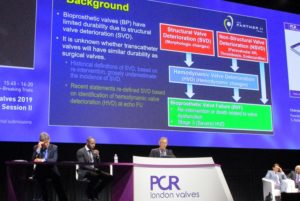
Pibarot outlined the rationale behind the analysis: “Bioprosthetic valves have limited durability due to structural valve deterioration (SVD). It is unknown whether transcatheter valves will have similar durability to surgical valves. Historical definitions of SVD, based only on reinterventions, grossly underestimated the incidence of SVD, and so recent statements redefined SVD based on the identification of haemodynamic valve deterioration (HVD) at echo follow up. Haemodynamic valve deterioration may lead to bioprosthetic valve failure … and may be caused by structural valve deterioration, but also by non-structural valve deterioration, which includes paravalvular aortic regurgitation thrombosis and endocarditis.”
The analysis focused primarily on SVD and aimed to determine the incidence of SVD-related HVD and/or BVF at four to five years of follow up after TAVI and surgery in intermediate-risk patients from the PARTNER 2A trial and registry. It looked at both arms of the PARTNER 2A randomised trial (Sapien XT vs surgery, n = 2,032), and the PARTNER 2 Sapien 3 intermediate-risk registry (n=1,078). Only patients who had their valve implanted (valve implanted [VI] population) were included in the analysis.
HVD was graded as stage one (morphological valve leaflet changes only), two (moderate HVD), or three (severe HVD). The annual rates of HVD and/or BVF were reported as rate per 100 patient–year exposure. Five-year (four-year for Sapien 3) cumulative rates of HVD and/or BVF were reported as Kaplan Meier curves for all cohorts. Investigators then compared PARTNER 2A Sapien XT vs. surgery and PARTNER 2 Sapien 3 intermediate vs. PARTNER 2A surgery using the hazard ratio (HR) log rank test.
In the surgical arm of the VI population (n=936), 17 cases of SVD-related HVD were identified and three cases of SVD-related BVF. Among 974 Sapien XT patients, there were 45 SVD-related HVD cases and 18 SVD-related BVF. And in the Sapien 3 intermediate-risk registry (n=1,069) there were 21 cases of SVD-related HVD, and four of SVD-related BVF.
The hazard ratio for SVD-related HVD was 0.41 (95% confidence interval [CI] 0.23 to 0.74, p=0.002) at five years in Sapien XT vs. surgery, and 0.93 (95% CI 0.44-1.98, p=0.86) at four years in Sapien 3 vs. surgery.
Pibarot said: “The rate of SVD-related HVD was significantly higher in the Sapien XT arm versus the surgical arm. However, the rate in the S3i registry was similar to surgery. The rate of SVD-related BVF was significantly higher in Sapien XT versus surgery [at five years]; whereas the rate in the S3i [Sapien 3 intermediate-risk patients] at four years was similar to that of surgery and not statistically significant.”
A composite to the two endpoints demonstrated a significantly higher rate of Sapien XT vs. surgery and similar rates in Sapien 3 intermediate-risk patients and surgery.
Secondary endpoints for bioprosthetic valve failure related to SVD or non-structural valve deterioration, also showed higher rates for Sapien XT than surgery. “In S3i, numerically there were more all-cause BVF at four years but this was not statistically significant compared to surgery.”
The majority of causes of bioprosthetic valve failure in the surgical arm were related to endocarditis (50%), followed by SVD (37.5%). In the Sapien XT cohort, most failures were due to SVD (66.7%) with 18% due to paravalvular regurgitation. In patients receiving the Sapien 3 valve, most cases of failure were caused by paravalvular regurgitation (64.7%).
Mortality at 30-days related to reintervention was high (50%) in the surgery arm, and significantly higher versus the 5% among those receiving Sapien XT, and zero in the Sapien 3 cohort.
Limitations were that randomisation was available only for Sapien XT vs. surgery comparison but not for that between Sapien 3 and surgery, and that five-year follow up was not available for Sapien 3 intermediate-risk patients.
Pibarot said: “On the basis of these results, I would like to conclude that the second generation of Sapien transcather valve—Sapien XT—has lower midterm durability compared to surgery whereas the third generation—Sapien 3—has similar durability.”
He added: “We will do a stratified analysis in each cohort to determine the baseline factors associated with SVD. These factors may be indeed be different in surgery vs. TAVI XT vs. TAVI S3.”









