
Telemedicine has come into its own during the pandemic. Sameer Mehta details the STEMI treatment strategy of the Latin America telemedicine infarct network (LATIN), and shares lessons learnt.
The response to the coronavirus pandemic has led to seismic developments around the use of telemedicine, as its capabilities for optimising healthcare are illustrated and its various attributes become more apparent. After the pandemic recedes, there will not necessarily be a reduction in the popularity of telemedicine. On the contrary, we may find ourselves using it even more to flatten disparities of care and to deliver cost-effective healthcare beyond geographical boundaries.
The work of Latin America telemedicine infarct network (LATIN) provides valuable lessons about the power of telemedicine and its potential for efficient management of population-based conditions, such as acute myocardial infarction (AMI).
The size of LATIN is unprecedented, and the subjects treated in the programme easily exceed the combined numbers in all other reported telemedicine trials. LATIN has cared for almost 900,000 patients, whereas the next biggest telemedicine network (Apulia, Italy) has managed 51,000 patients. The 355 LATIN centres provide an umbrella of AMI care to >100 million patients (Figure 1), all of whom received telemedicine-guided access to world experts and to a guidelines-based AMI programme of early reperfusion.

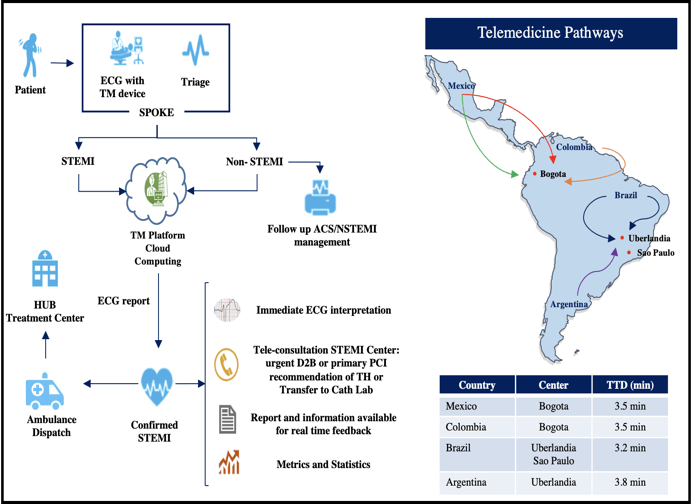
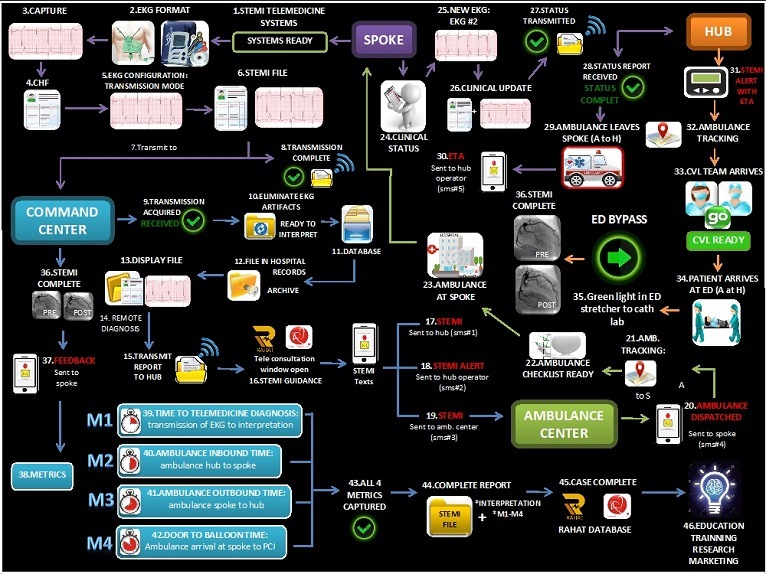
LATIN uses a “hub and spoke” strategy, and the protocol of AMI care involves urgent reperfusion of patients with thrombolysis, pharmacoinvasive management, or primary percutaneous coronary intervention (PCI). The “spokes” are located in remote regions, often up to 200 miles from the “hubs”, where primary PCI is performed. Expert cardiologists located at command centres use sophisticated telemedicine platforms to immediately interpret an electrocardiograph (ECG) and to guide the entire AMI triage and treatment strategy.
LATIN was first launched as a pilot programme in 2012 in Barranquilla, Colombia. This helped to highlight the various challenges—technology gaps, cultural barriers, infrastructure deficits, ambulance shortages, lack of PCI facilities, and reimbursement issues. As the programme was expanded to other cities in Colombia, and later to Brazil, Mexico, and Chile, these challenges were gradually overcome, apart from the issue of payment for the procedures—this was beyond the scope of LATIN and was related to numerous healthcare reimbursement and funding issues. Not unexpectedly, we confronted enormous regional variability in all of the four countries, and the programme was forced to adapt to the changing landscape by triaging to local treatment modality and to the availability of ambulances and 24/7 PCI treatment.
Almost 900,000 patients have received telemedicine guidance at 355 centers that employ standardised protocols and telemedicine guidance; 72% were treated with primary PCI, and door to balloon (d2b) times were 48 minutes. In-hospital mortality was 5.2%, a 55% overall reduction compared to a historic cohort. Time to telemedicine diagnosis (TTD) was formulated as a metric to monitor telemedicine efficiency (Figure 2), and it included the transmission of the ECG from the spoke, elimination of artefacts and incorporation within HIPAA (Health Insurance Portability and Accountability Act of 1996) guidelines, interpretation by the expert at the telemedicine centre, notification of diagnosis to the spoke, and alerts that were simultaneously issued for the spoke, the hub, and for ambulance dispatch.
A mean TTD of 3.5 minutes was achieved, both in the sites that were guided from within the country (Colombia and Brazil) and those guided from outside the country (Mexico and Argentina). Achieving telemedicine efficiency with such low TTD required tremendous expert commitment, meticulous on-site training, and investments in cloud computing and the design of high fidelity telemedicine platforms.
Considerable savings accrued from avoiding unnecessary transfer and treatment, and by early hospital discharge and reduced medications. Figure 3 is an economic forecast of LATIN that demonstrates the incremental cost savings from the programme.

There have been numerous gains from the LATIN program—directly, as evidenced by the lives saved and from the cost-savings, and also from the halo effect of LATIN. Before the programme was initiated, policy for AMI care in Central and South America was ad hoc, with scattered centers of excellence and most patients either getting no or delayed perfusion with first generation lytics. Urgent triage and transportation were rare and d2b times virtually unheard of. There were no community awareness programmes about the need for and availability of primary PCI. After almost a decade of LATIN, stakeholders have been broadened, ST elevation myocardial infarction (STEMI) networks have become available, ambulance structure has significantly improved, and patient awareness is better. At the first LATIN pilot site in Barranquilla, before the programme, 80% of patients self-transported to either the spoke or the hub and presented 7.1 hours after chest pain. Presently, almost all are being transported by ambulance, and 79% are being treated with primary PCI with short d2b.
We believe LATIN provides a cost-effective template for reducing disparities of AMI care and that its greatest relevance is in poor regions of the world, including in SE Asia, the Middle East and Africa. Figure 4 demonstrates a straightforward application of LATIN in India, with the RAHAT heart attack programme that provides AMI management to 65 million patients in India’s largest state of Rajasthan.
In addition to expanding to other parts of the world, there appear to be four future applications:
- telemedicine guided programmes for other time-dependent clinical entities, such as stroke. LATIN telestroke is testing a pilot programme;
- integrating telemedicine and artificial intelligence (AI) into a seamless, physician-free management of AMI systems of care;
- impacting symptom to balloon times with self-administered AI guided tools for AMI detection that are embedded into telemedicine protocols. We are presently testing a single lead, AI algorithm at LATIN sites;
- remote primary PCI with platforms such as Corindus.
Sameer Mehta is the chairman of the Lumen Foundation in Miami, USA










