By Daniel Steinberg
Daniel Steinberg reviews the transradial approach in primary percutaneous coronary intervention (PCI) and looks at why the USA has been reluctant to adopt the approach despite it reducing access site and bleeding complications compared with the transfemoral approach
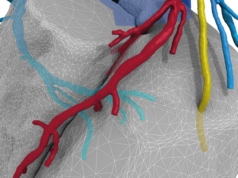
It has been almost a quarter of a century since the early reports describing transradial catheterisation and percutaneous coronary intervention (PCI) were published. Over this span, a consistent message has emerged: transradial access, though technically more challenging, reduces access site and bleeding complications compared with the transfemoral approach. With refined technique and improved equipment, it has seen a gradual wave of interest, enthusiasm and uptake across the world.
In some countries, it is more common than transfemoral access for patients undergoing PCI.
However, the interventional community in the USA has been somewhat slow to adopt transradial intervention. The reasons for this are complex, but they largely relate to a lack of dedicated training, steep learning curves, and a natural human resistance to change. While there is little debate that access site bleeding is decreased with transradial intervention, the RIVAL trial results suggested similar rates of death, myocardial infarction, stroke and major bleeding with each approach1.
These findings fuelled the argument that the approach is not necessarily worth the increased procedural time, radiation exposure and conversion rates necessary to overcome the initial learning curve. Although the debate continues, training efforts through industry and the societies have resulted in increased transradial use across the USA.
Of particular interest are a number of recently published studies suggesting a significant mortality benefit of transradial intervention in patients presenting with ST-segment elevation myocardial infarction (STEMI). These include the STEMI subset of the randomised RIVAL (n=1,958)2 and RIFLE-STEACS (n=1,001)3 studies, and the observational Cath-PCI registry (n=90,879)4. Each demonstrated a statistically significant 36–60% relative mortality reduction with transradial intervention compared to transfemoral primary PCI. Importantly, improved outcomes were noted despite a small increase in door-to-device times. Although vascular complications were clearly lower in patients treated via transradial primary PCI, bleeding rates were lower only in RIFLE-STEACS and the Cath-PCI registry, but not in RIVAL. This finding suggests that additional unmeasured factors may contribute to the benefit of transradial primary PCI.
It is worth reiterating that door-to-device times were slightly higher in the transradial approach, but mortality was still lower than that with transfemoral access. Over the past decade, the primary focus in STEMI has been rapid access to the catheterisation laboratory to open the occluded artery as fast as possible. The interventional community has been tremendously successful in this regard, but mortality is relatively stable over the past few years. Possibly, we have hit a plateau in effectiveness, and a shift toward improved safety (ie. reduced bleeding complications) may be the next frontier.
As evidence supporting mortality benefit with transradial intervention in STEMI continues to mount, we are left wondering whether these studies will lead to further uptake of transradial intervention. The Cath-PCI registry suggests that such change is occurring. From 2007 to 2011, transradial primary PCI increased from less than 1% to 6.8%, and these numbers are gradually continuing to climb. Perhaps the message is already communicated, and time alone will lead to evolution of practice. Also probable, continual changes in the healthcare landscape such as those regarding reimbursement for preventable complications or pressures to decrease costs will fuel further change.
The largest impediment to routine transradial primary PCI in the USA is the learning curve associated with the procedure itself. As the societies continue to embrace transradial PCI and the academic centres begin to teach the radial artery as default access instead of a niche technique, comfort with transradial access should continue to improve. Along with the body of evidence supporting clinical benefit of transradial intervention, especially in the setting of STEMI, increased comfort with transradial techniques will inevitably lead to increased use. Ultimately, it is probable that transradial access will become the default strategy in primary PCI.
Daniel H Steinberg is assistant professor of Medicine, Interventional Cardiology, Medical University of South Carolina, Charleston, USA
Conflict of Interest: consultant for Terumo Interventional Systems, Boston Scientific, Medtronic, St Jude, Astra Zeneca
References
1. Jolly et al. Lancet 2011; 377:1409–20
2. Mehta et al. J Am Coll Cardiol 2012; 60:2490–99
3. Romagnoli E et al. J Am Coll Cardiol 2012; 60: 2481–89
4. Baklanov et al. J Am Coll Cardiol 2013; 61:420–26