A new study indicates that “transcatheter valve-in ring”—implanting a transcatheter valve in a surgically placed annuloplasty ring—may be a clinically effective approach for managing tricuspid regurgitation in previously treated patients. However, investigators Jamil Aboulhosn (David Geffen School of Medicine at UCLA, Division of Cardiology, UCLA, Los Angeles, USA) and others found that paravalvular leak was common after the procedure and may lead to further interventions.
Writing in JACC: Cardiovascular Interventions, Aboulhosn et al report that the longevity of surgical repair, with an annuloplasty ring, of tricuspid regurgitation “remains suboptimal”—commenting that “more than 25% of patients” develop progressive moderate or severe tricuspid regurgitation within five years or repair “depending on various clinical and technical factors”. They add that patients with failing annuloplasty rings are often complex and have numerous comorbidities, making them “at high risk for adverse outcomes” after tricuspid valve reoperation. For this reason, the authors note, off-label transcatheter valve-in-ring procedures are an “appealing alternative” to re-do surgery. Therefore, given “little is known” about the results of transcatheter valve-in-ring procedures, Aboulhosn et al reviewed data collected from a registry of institutions that have performed such procedures.
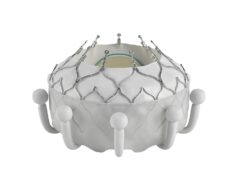
Of 22 tricuspid regurgitation patients scheduled to undergo transcatheter valve-in-ring implantation, two did not receive the procedure; based on the results of balloon testing, these patients had no appreciable landing zone or tricuspid regurgitation through the open portion of the annuloplasty ring. The authors write: “All procedures were performed under general anaesthesia, mostly from a femoral venous approach (73%) with transoesophageal echocardiographic guidance. A Sapien valve was implanted in 17 patients (85%)—most often a 26mm or a 29mm Sapien XT (80%)—and a Melody valve were implanted in three.”
Prior to undergoing transcatheter valve-in-ring implantation, all patients had moderate or severe tricuspid regurgitation and four had significant tricuspid stenosis. Afterwards, no patients had tricuspid regurgitation or stenosis. Additionally, the mean right atrium–right ventricle gradient ranged from 0 mmHg to 5mmHg. However, Aboulhosn et al state, four patients required reintervention during the index procedure because of paravalvular leak—with one undergoing additional transcatheter valve-in-ring implantation and three receiving an occlusion device. “One patient with paravalvular leak underwent surgical tricuspid valve replacement six days post transcatheter-in-valve implantation,” they add.
Although paravalvular leak was common and occurred in 75% of patients, at the latest follow-up point (median 12 months), no patients had more than mild tricuspid regurgitation. Improvement in functional capacity was seen in the majority of patients—the median New York Heart Association (NYHA) functional class was III prior to procedure and was II after the procedure. However during follow-up, Aboulhosn et al report that a 75-year-old man died “despite a successful transcatheter valve-in-=ring implantation and closure of a moderate paravalvular leak with two occluders”. They add, in addition to two patients who received a second transcatheter valve-in-ring implantation during the index procedure, one other patient underwent a repeat transcatheter valve-in-ring during follow-up. “Fifteen months after the original procedure, a 29mm Sapien XT valve was placed for persistent paravalvular leak, but there was still residual paravalvular leak, so a third transcatheter valve-in-ring implantation was performed 10 months later (29mm Sapien 3 device) along the placement of muscular vascular septal defect occluder. Soon after this, the patient developed haemolysis and severe tricuspid stenosis, so surgical tricuspid valve replacement was performed,” the authors write.
Aboulhosn et al note that transcatheter valve-in-ring implantation is “more challenging” than transcatheter valve-in-valve implantation “due to the larger diameters and geometric variability of surgically placed rings”. They add that “incomplete rings, which were present in all but one patient, are most challenging because a circumferential landing zone is not available and therefore, the risk of valve embolisation and paravalvular regurgitation is higher”.
Aboulhosn told Cardiovascular News: “The use of commercially available transcatheter valve platforms to perform non-surgical transcatheter tricuspid valve in ring replacement fulfils a clinical need in this unique population. This study demonstrates the efficacy and safety of transcatheter valve-in-ring. It should be noted that paravalvular regurgitation is commonly encountered post transcatheter valve-in-ring and can be effectively treated with transcatheter device occlusion.”