A retrospective economic analysis of the LIFE-BTK trial has demonstrated the one-year cost-effectiveness of an everolimus-eluting resorbable scaffold over angioplasty for the treatment of infrapopliteal artery disease, with investigators predicting more significant results in the longer term.
Sharing this finding at TCT 2024 (27–30 October, Washington, DC, USA), LIFE-BTK co-principal investigator Sahil Parikh (Columbia University Irving Medical Center, New York, USA) highlighted a “significant difference” in terms of one-year cost-effectiveness in favour of the Esprit BTK resorbable scaffold (Abbott Vascular) over angioplasty using a “relatively modest” willingness-to-pay threshold.
These data come one year after the presentation and simultaneous publication of first results from the LIFE-BTK trial, which enrolled 261 patients globally at 50 sites. The headline finding, Parikh summarised, was that 74.5% of the Esprit BTK group achieved a composite endpoint of limb salvage and primary patency versus 43.7% of the angioplasty group.
With these data in hand, the LIFE-BTK leading investigators—namely Parikh, Ramon Varcoe (Prince of Wales Hospital and University of New South Wales, Sydney, Australia) and Brian DeRubertis (New York Presbyterian–Weill Cornell Medical Center, New York, USA)—set out to perform a cost-effectiveness analysis.
The investigators considered the costs of index procedure and follow-up visits (inpatient, outpatient and office), as well as the incremental cost-effectiveness ratio (ICER)—defined as the difference in total costs divided by the difference in primary endpoint failure or clinically driven target lesion revascularisation (CD-TLR).
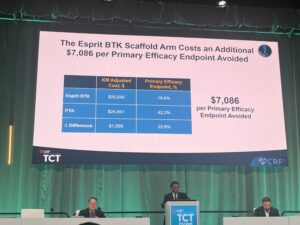
At TCT 2024, Parikh shared that index costs were not statistically significant between the Esprit BTK and angioplasty groups, and that follow-up costs were similarly well matched. “The total difference in costs was modest,” he said, citing a gap of less than US$2,000 between the two groups.
The presenter continued that, “using the most conservative delta between the two groups in terms of the primary efficacy endpoint at 365 days, not inclusive of the treatment window”, the Esprit BTK scaffold costs an additional US$7,086 per primary efficacy endpoint avoided.
This led Parikh to report that the Esprit BTK scaffold achieves a 64% probability of cost-effectiveness at a US$10,000 willingness-to-pay threshold compared to angioplasty. As a result of this, he averred: “The use of Esprit BTK at one year alone is likely to be cost effective.”
The presenter went on to note that that Esprit BTK scaffold costs an additional US$22,163 per CD-TLR avoided.
Parikh summarised that the Esprit BTK scaffold shows proven benefit in delaying the need for repeat revascularisation in patients with below-the-knee (BTK) disease and that cost-effectiveness is “likely to increase over time if the reduction of TLR remains consistent over time”.
Additionally, the presenter stressed that the Esprit BTK scaffold is the only US Food and Drug Administration-approved option for patients with chronic limb-threatening ischaemia (CLTI) and infrapopliteal artery disease.
Looking ahead, Parikh highlighted the upcoming presentation of two-year LIFE-BTK results, which DeRubertis is set to announce this week at VIVA 2024 (3–6 November, Las Vegas, USA).












