Five-year data from the PARTNER 3 trial, which randomised low surgical risk aortic stenosis patients to receive either transcatheter aortic valve implantation (TAVI) with the Sapien 3 (Edwards Lifesciences) device or surgery, has continued to show equivalent performance between the two treatments against its composite endpoint of death, stroke or rehospitalisation.
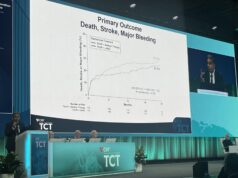
However, reporting the findings at TCT 2023 (23–26 October, San Francisco, USA), PARTNER 3 investigator Marty Leon (Columbia Irving Medical Center/New York Presbyterian, New York, USA) noted that there was an attenuation of the differences between the two groups in the primary endpoint out to five years, which had initially favoured TAVI at both one and two years.
The trial enrolled 1,000 patients with severe symptomatic aortic stenosis between March 2016 and October 217 to undergo TAVI using the Sapien 3 balloon-expandable valve (n=503) or surgery (n=497) for severe aortic stenosis.
The trial’s results at one and two years demonstrated superior or similar results for TAVI for the primary endpoints of death, stroke or rehospitalisation, Leon said in his presentation. As the majority of aortic stenosis patients treated with surgery have low surgical risk profiles and are younger, the five-year outcomes from PARTNER 3 are essential to inform patient-centred therapy for initial and subsequent aortic valve procedures, Leon said.
Presenting the primary endpoints at five years, Leon reported a non-hierarchical composite of all-cause death, all stroke, or rehospitalisation of 22.8% in the TAVI arm, versus 27.2% in the SAVR arm, a narrowing of the difference seen between the two therapies from the trial’s earlier results.
In the TAVI arm, all-cause mortality was 10%, cardiovascular mortality was 5.5% and disabling stroke was 2.9% at five years. Leon pointed out that there were similar rates of cardiovascular death in both arms, but noted that there was a higher prevalence of non-cardiovascular death in the patients who received TAVI.
Rehospitalisation was less than 3% per year over five years. Valve durability indicators were also stable over time with no difference in the incidence of bioprosthetic valve failure related to structural valve deterioration (1.4% vs. 2%) or reintervention rates (2.6% vs. 3%) between TAVI and surgical aortic valve replacement (SAVR).
Analysis of five-year data from the trial found that rates of all-cause mortality, disabling stroke and rehospitalisation remained low and all secondary endpoints were consistent with the surgical control arm.
According to Leon, the five-year findings from the trial reaffirm the clinical and echocardiographic benefits of TAVI with the Sapien 3 valve as a meaningful alternative to surgical therapy for low-risk severe, symptomatic AS patients.
“The five-year follow-up findings from the PARTNER 3 trial reaffirm the clinical outcome benefits and bioprosthetic valve durability of Sapien 3 TAVI as a meaningful alternative to surgical therapy for low-risk severe, symptomatic aortic stenosis patients,” said Leon.