The first randomised trial to compare the safety and efficacy of the Acurate neo transcatheter heart valve (Boston Scientific) with the Sapien 3 TAVI device (Edwards Lifesciences) did not meet non-inferiority in patients with severe aortic stenosis.
The findings were reported today at the 31st Transcatheter Cardiovascular Therapeutics scientific symposium (TCT 2019; 25–29 September, San Francisco, USA), and simultaneously published in The Lancet. Investigator Jonas Lanz (Bern University Hospital—Inselspital, Bern, Switzerland) told delegates that the differences between the two TAVI devices were “driven by moderate or severe paravalvular regurgitation and stage 2 or 3 acute kidney injury, in favour of the Sapien 3 device”.
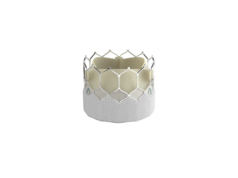
In a roundtable discussion that followed the presentation, Martin B Leon (Columbia University Medical Center, New York, USA) said he was “impressed that the supra-annular expanding device shows very good haemodynamics”, and expressed confidence that once the next-generation of the device, Acurate neo 2, is involved in clinical trials, and physicians have had the opportunity to use it in the USA “we will see these data change significantly”. “Many times you are dealing with devices in evolution. And we are aware that the Acurate neo is the first version of the Acurate neo—there is another version that is designed to reduce paravalvular leaks.”
Between February 2017 and February 2019, 739 patients with severe, symptomatic aortic stenosis at increased surgical risk were randomised 1:1 to transfemoral TAVI with the Acurate neo (n=372) or Sapien 3 (n=367) system at 20 European sites. Clinical follow-up information at 30 days was available for 98.9% and echocardiographic follow-up for 98% of the total study population.
SCOPE I was an investigator-initiated study designed to investigate non-inferiority of the primary endpoint, which was a composite of safety and efficacy derived from the Valve Academic Research Consortium-2 criteria and included all-cause death, any stroke, life-threatening or disabling bleeding, major vascular complications, coronary artery obstruction requiring intervention, acute kidney injury ≥stage 2, valve-related dysfunction requiring repeat procedure, rehospitalisation for valve-related symptoms or congestive heart failure, moderate or severe prosthetic valve regurgitation or prosthetic valve stenosis at 30 days.
The primary endpoint rate in the intention-to treat cohort for Acurate neo was 23.7% compared to 16.5% with Sapien 3 (p noninferiority=0.42, which did not meet non-inferiority). Lanz also outlined that there were higher rates of multiple valve implantation in the Acurate neo arm. Transvalvular gradients were lower and effective orifice area larger with Acurate neo. Rates of mortality, stroke and pacemaker implantation were low with both devices.
Lanz listed the limitations of the trial, which included that it was not powered for individual clinical endpoints and that the early primary endpoint limits evaluation of device differences in terms of long-term clinical outcomes. Additionally, visible differences in the stent frame precluded blinding of the echocardiography core laboratory.
Responding to a question from the panel, Lanz said “I think we can assume that the difference would be different if we were comparing it to another self-expanding device”, and he revealed: “This is actually going to be addressed in the SCOPE II trial, led by another team, which will have a one-year endpoint that will compare Acurate neo versus CoreValve Evolut R [Medtronic].
And he pointed out: “The technological refinement that was made in the iteration with the [Acurate] neo 2 actually addresses paravalvular regurgitation,” he said, adding that the new valve will be assessed in trials against other commercially available devices. Among other factors to be considered are “whether there are anatomical features which predispose, and whether there is an issue with undersizing”.