By Tim Kinnaird
Despite its relative infrequency, stent thrombosis has devastating outcomes for patients; therefore, its avoidance is a major driver of improving interventional technique, the use of pharmacological therapies, and ongoing research. While the first iteration of drug-eluting stents—such as the paclitaxel-eluting stent Taxus (Boston Scientific) and the sirolimus-eluting stent Cypher (Cordis)—effectively suppressed restenosis (compared with bare metal stents), they were associated with incidences of late and very late stent thromboses (at even seven years after implantation).
In a postmortem study, Renu Virmani’s group identified that the completeness of the endothelial coverage of stent struts was the most powerful predictor of late stent thrombosis.1 This observation is consistent not only with the pathophysiology of thrombosis and poor healing (with the continued exposure of polymer and metal to circulating coagulants), but also with the postulated mechanism of neoatherosclerosis. This recently described pathological process is proposed to occur when an incomplete endothelial barrier is present, resulting in the unobstructed passage of lipids and macrophages into the sub-intima leading to the rapid accumulation of new plaque.2 Therefore, late and very late stent thrombosis may occur partly through thrombosis and also partly through plaque rupture in neoatherosclerosis.
However, in both events, incomplete endothelialisation is the common pathological theme.
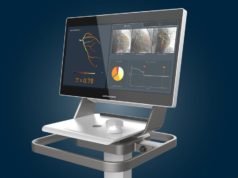
As part of these pathological studies, Virmani’s group also identified the ratio of covered to uncovered struts as the best morphometric surrogate for late stent thrombosis and recent data confirs the ability of optical coherence tomography (OCT) to measure this pathological parameter. The extremely high resolution of OCT (10–20μm) allows clear visualisation of stent struts and overlying neointima, and OCT is increasingly being used in clinical practice and research studies to optimise stent implantation, assess healing and interrogate mechanisms of stent thrombosis and restenosis. For example, in an animal model, OCT correlated very closely with histological measures of stent performance with extremely high I2 values for stent area, area stenosis, percentage of uncovered struts and neointimal area.3
The imaging modality, therefore, provides clinicians and researchers alike with the opportunity to compare the healing properties of conventional stents. A human study showed that a biolimus-eluting stent was associated with a significant reduction in the number of covered struts, as assessed by OCT, compared with a sirolimus-eluting stent at six-month post-implantation (15.9% vs. 25.1%, respectively).
OCT also provides the ability to assess healing in new stent technologies of interest. Of particular relevance in the sphere of optimal healing is the Combo dual therapy stent (OrbusNeich). This stent combines the luminal anti-CD34+ antibody capture technology, first seen with the Genous stent, with the abluminal release of sirolimus from a fully absorbable polymer. As well as the sirolimus-mediated suppression of smooth muscle cell proliferation, it is proposed that—as a result of the CD-34+ antibody—rapid endothelialisation will also occur. This hypothesis has been examined in several animal models and the proposed healing characteristics have been observed as predicted.5 After encouraging first-in-man studies of Combo, the stent is now rapidly moving into the clinical arena with several large on-going randomised trials and registries. Most recently, a clinical OCT study has confirmed the encouraging healing data derived from animal models. In the EGO-COMBO studies, patients underwent serial OCT imaging at a variety of time points up to 24 months after implantation of the Combo stent.6 This study demonstrated very rapid endothelialisation of the stent, which resulted in almost complete strut coverage at five months—an observation that compares extremely favourably with OCT interrogation of first- and second-generation stents.3
Data suggest that incomplete stent strut coverage is the most important predictor of late thrombosis and that OCT can reliably measure this parameter. Newer stent technologies, such as the Combo stent, when interrogated by OCT, appear extremely encouraging. Ongoing clinical trials are addressing the issue of whether these surrogates of healing will translate into superior clinical outcomes.
References
- Finn et al. Circulation 2007; 115: 2435–41.
- Nakazawa et al. J Am Coll Cardiol 2011; 57: 1314–22.
- Malle et al. ATVB 2013; 33: 1376.
- Kim et al. Eurointervention 2014; 9: 1389–97.
- Granada et al. Circ Cardiovasc Interv 2010; 3: 257–66.
- Lee. TCTAP 2014
Tim Kinnaird, Department of Cardiology, University Hospital of Wales, Cardiff, Wales