Of 5,691 adverse events following transcatheter aortic valve implantation (TAVI) that were reported to the FDA’s manufacturer and user facility device experience (MAUDE) database, only 30 related to clinical or symptomatic leaflet thrombosis. However, these events were associated with serious clinical manifestations including stroke, cardiogenic shock, and death.
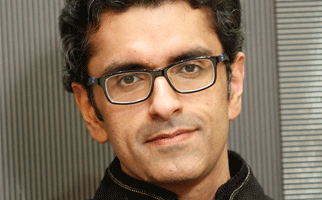
Abdul Moiz Hafiz (Southern Illinois University School of Medicine, Springfield, USA), Ankur Kalra (Harrington Heart & Vascular Institute, University Hospitals Cleveland Medical Center, Cleveland, USA), and others write in Structural Heart that leaflet thrombosis after TAVI is recognised as “a relatively novel and important mechanism” of transcatheter heart valve failure. They add that while previous studies have provided some information on the complication, data are still lacking. “Whether clinically manifest leaflet thrombosis has significance beyond peri-TAVI stroke or transient ischaemic attacks is yet to be elucidated. Specific possibilities include premature structural valve degeneration, central aortic regurgitation, recurrent heart failure, or increased risk of sudden death,” Hafiz, Kalra, et al comment.
Therefore, the authors “interrogated the MAUDE database to investigate the frequency, management, and outcomes of TAVI-related adverse events due to clinical or symptomatic leaflet thrombosis.” Of 5,691 TAVI-related adverse events that were recorded in the database, after procedural events and those of unknown cause were excluded, 156 were found to be related to structural valve dysfunction. Of these, 129 were categorised as leaflet restriction and 27 were categorised as leaflet malcoaptation. Overall, 30 were identified as being caused by leaflet thrombosis—20 with a Sapien valve (Edwards Lifesciences) and 10 with a CoreValve device (Medtronic).
According to Hafiz, Kalra, et al, most cases (60%) of leaflet thrombosis occurred within the first year of TAVI. They add that the structural valve dysfunction manifested as aortic stenosis (16), aortic regurgitation (7), or both (4). The remaining three cases were associated with clinically manifest stroke or transient ischaemic attack. The authors report: “Interventions to address leaflet thrombosis included either escalation of antiplatelet or anticoagulation therapy (30%), valve-in-valve TAVI (16.7%), surgery (46.7%), or their combination.”
Hafiz, Kalra et al comment that “although infrequently reported,” clinically manifest leaflet thrombosis was associated with a “poor prognosis.” They note that three patients experienced a stroke/transient ischaemic attack, two patients experienced cardiogenic shock, and nine patients died. “Death occurred in seven of nine cases despite interventions to address clinical leaflet thrombosis,” the authors observe.
Concluding, they state: “As indications for TAVI expand to include patients at intermediate and perhaps low risk for perioperative mortality following surgery, an early diagnosis of leaflet thrombosis may be crucial for planning appropriate management and optimising clinical outcome of this patient subset.”
Coinciding with its publication in Structural Heart, the study was also presented at the European Society of Cardiology (ESC) congress (26–30 August, Barcelona, Spain). Speaking at the ESC congress, Kalra commented: “While these data do not provide the frequency of these events [overall], and undoubtedly the clinical events often led to the recognition of leaflet thrombosis, they are useful in that establish definitive evidence of its occurrence.”
Talking to Cardiovascular News about how leaflet thrombosis should be identified and managed, he said: “It is currently not known how frequently to obtain follow-up echocardiograms on patients following TAVI. If a follow-up echocardiogram demonstrates elevated mean gradient, one of the differentials to think about is leaflet thrombosis. This should be further investigated by either a transoesophageal echocardiogram or volume-rendered computed tomographic reconstruction. Management includes initiating anticoagulation with either warfarin or direct oral anticoagulants.”