Eight-year findings from the NOTION I trial—the first all-comers trial to randomise low-risk patients to transcatheter aortic valve implantation (TAVI) or surgical aortic valve replacement—were presented during a late-breaking trial session at PCR Valves e-course (22–24 November, virtual). NOTION I showed that at eight years, patients undergoing TAVI had a comparable rate of all-cause mortality and stroke compared to those receiving a surgical procedure.
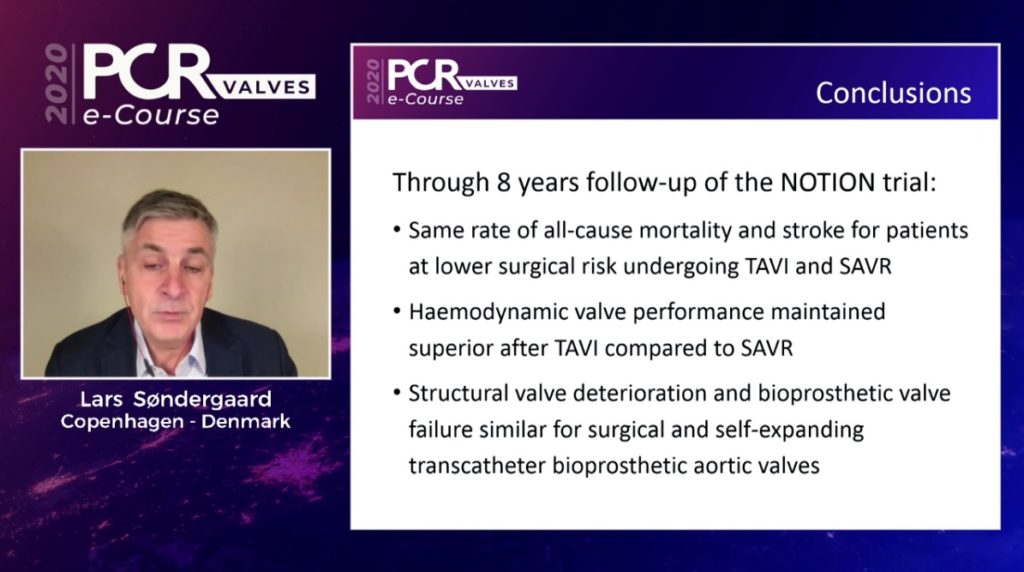
The findings, presented by Lars Søndergaard (The Heart Centre, Rigshospitalet, Copenhagen, Denmark), also showed that haemodynamic valve performance maintained superiority after TAVI compared to surgical valve replacement, and that structural valve deterioration and valve failure were similar in both groups.
NOTION I, conducted at centres in Denmark and Sweden, enrolled patients between 2009–2013 who were suitable for both TAVI and surgical valve replacement. Patients were required to be 70 years or older for inclusion in the trial. Those undergoing TAVI received the first-generation Corevalve (Medtronic) prosthesis.
The study had primary endpoint of composite all-cause mortality, stroke or myocardial infarction after one year. In total 280 patients, with a mean age of 79 years, were randomised to receive TAVI or surgical intervention. “Society of Thoracic Surgeon’s (STS) score was what we would call low, and mean STS score around 3%. More than 80% had an STS score of less than 4%,” Søndergaard said in his presentation.
About half of the patients are still alive after eight years, and there is no difference between patients undergoing a transcatheter or surgical aortic valve replacement, Søndergaard told PCR Valves attendees.
“If you look at the initial primary composite endpoint of all-cause mortality, stroke and myocardial infarction, there is still no difference between these endpoints with transcatheter and surgical aortic valve replacement,” Søndergaard commented. “We also looked at the haemodynamic performance, and maybe not surprisingly in self-expanding transcatheter aortic valves, [with] the supra-annular position of the leaflets of the CoreValve, you get a better performance with a higher opening area and lower mean gradient than the surgical valve and that is sustained out to eight years.”
Discussing the durability of the transcatheter valves, Søndergaard acknowledged that this has been an area of significant debate, but noted that there is now a European consensus document on valve (published in 2017 in the European Heart Journal and European Journal of Cardiothoracic Surgery) which defines valve durability using both bioprosthetic valve dysfunction (comprising of structural valve deterioration, non-structural valve deterioration, and bioprosthetic valve thrombosis/endocarditis) and bioprosthetic valve failure (valve-related death, aortic valve reintervention, and severe haemodynamic structural valve dysfunction).
“Maybe the most important factor for valve dysfunction is structural valve deterioration, defined as a mean gradient of 20mmHg or more, a step-up in mean gradient of at least 10mmHg, or moderate or severe intra-prosthetic aortic regurgitation.
“You may argue this does not take patient prosthesis mismatch into account, so if you try to modify these criteria and say that patients need to have a gradient of at least 20mmHg and a step up in gradient of at least 10mmHg, it is going to counterbalance the risk of including patients with a prosthesis mismatch.”
Looking at patients based solely upon the 2017 European consensus document, Søndergaard said, “you can see at eight years there are twice as many patients who had the surgical repair” (28.5% vs. 14.1%).
Using the modified criteria, requiring both a high gradient and an increase of the gradient of at least 10mmHg, Søndergaard noted that this indicated no statistical difference between the two groups, despite the numerically lower rate of 9% in the transcatheter arm compared to 16% in the surgical arm.
“The European consensus report also defined valve failure as either due to valve-related death, aortic valve reintervention or severe haemodynamic structural valve deterioration,” Søndergaard added. “This means you have a gradient of at least 40mmHg or step up in gradient of at least 20mmHg, or severe aortic regurgitation.”
Applying this definition to the NOTION I data, at one-year Søndergaard revealed that there was no statistical difference between the two groups—7% for the transcatheter arm and 10% for the surgical arm.
Summarising the findings, Søndergaard said: “In this eight-year data from the NOTION I trial, you see the same rate of all-cause mortality and stroke for patients at lower surgical risk undergoing TAVI and surgical aortic valve replacement. Haemodynamic valve performance maintained superiority after TAVI compared to surgical valve replacement, using the Corevalve platform. Structural valve deterioration and bioprosthetic valve failure are similar for the surgical and self-expanding transcatheter heart valves.”
Following his presentation of the results, Søndergaard was questioned by session facilitators David Hidlick-Smith (Royal Sussex County Hospital, Brighton, UK) and Sabine Bleiziffer (Heart and Diabetes Center NRW, Bad Oeynhausen, Germany).
Hidlick-Smith posed a question about the life expectancy and major adverse events, and whether the data show and deviation from normal life expectancy within that age group.
Søndergaard responded that the research team had indeed investigated the outcomes of around 700 patients who underwent TAVI in the same era in Denmark, matching them to a control group with the same comorbidities, age and gender. “You can see after three months, these patients had the same mortality or survival rate as the general population,” he commented.
Bleiziffer questioned whether the trial results shed light on long-term valve-durability, and the decision between TAVI and surgical intervention in patients suitable for both approaches.
“First of all, when you talk about durability, and if we are going to look at patients with a much younger age we need longer follow-up than eight years, probably 10 or 15 years to prove that the durability is equal for these two valves,” Søndergaard commented. “But, I think it is reassuring that we can see here at eight years that the rate of heart valve failure is pretty low, around 10% for both arms, so I think that is reassuring that we do not see any short or intermediate term failure of these valves, which was a little bit of a concern in the beginning of the programme.”










