Long-term data on the outcomes of surgery after failed transcatheter edge-to-edge mitral valve repair, taken from the CUTTING-EDGE registry, were shared during a late-breaking trial session at PCR Valves 2020 (22–24 November, virtual). According to Gilbert Tang (Mount Sinai Health Sytem, New York, USA), who presented the data, CUTTING-EDGE is the first international registry to look at patients with degenerative and functional mitral regurgitation after transcatheter edge-to-edge repair.
“Over 100,000 transcatheter mitral valve edge-to-edge repair (TEER) have been performed worldwide, in patients with symptomatic moderate-severe to severe mitral regurgitation,” said Tang, in the introduction to his presentation, acknowledging, however, that longitudinal data on mitral valve surgery after transcatheter edge-to-edge repair is lacking.
CUTTING-EDGE looked at the differences between degenerative and functional MR patients in this cohort, Tang explained , describing the patient cohort as a highly selected group of patients, as it is not known the outcomes of patients for whom surgery was not performed.
In total data on 278 patients was collected through CUTTING-EDGE, from procedures performed at 27 centres around the world. “This is a long study. The first surgeries were done in 2009 with first MitraClip implanted in 2005, 15 years ago when MitraClip was first implanted, and as recently as this November,” Tang said.
Of the 278 patients from whom data were collected, the mean age was 73 years old, “a young group compared to most TAVI patients” Tang commented, with a median STS score of 5%. The majority were of procedures were performed with the original MitraClip (Abbott) valve, with degenerative/mixed disease in 55.7% of cases.
According to Tang, in around 16% of patients the transcatheter procedure was aborted, either in the same admission or subsequently. Furthermore, 18% were acute failure requiring surgery, and the majority of them around (66%) were delayed.
Outlining, the surgical indications, Tang detailed that recurrent MR was present in 39.7%, of patients who had subsequent surgery, leaflet detachment was noted in 34.2%, residual mitral regurgitation was identified in around 29% and mitral stenosis in 15.2%.
Mitral valve replacement was performed in almost all (95.6%) of these patients, with only a handful of them able to be repaired again, Tang noted, adding that 42.3% of these patients needed concomitant tricuspid surgery.
The mean cardiopulmonary bypass time was around 135 minutes and cross-clamp times were close to 1.5 hours. Tang revealed that 30-day and one-year mortality stood at 13.4% and 25.5% respectively, and added that surgery for recurrent mitral regurgitation was more frequent in degenerative disease (41.5% vs 23.7%) than in functional mitral regurgitation.
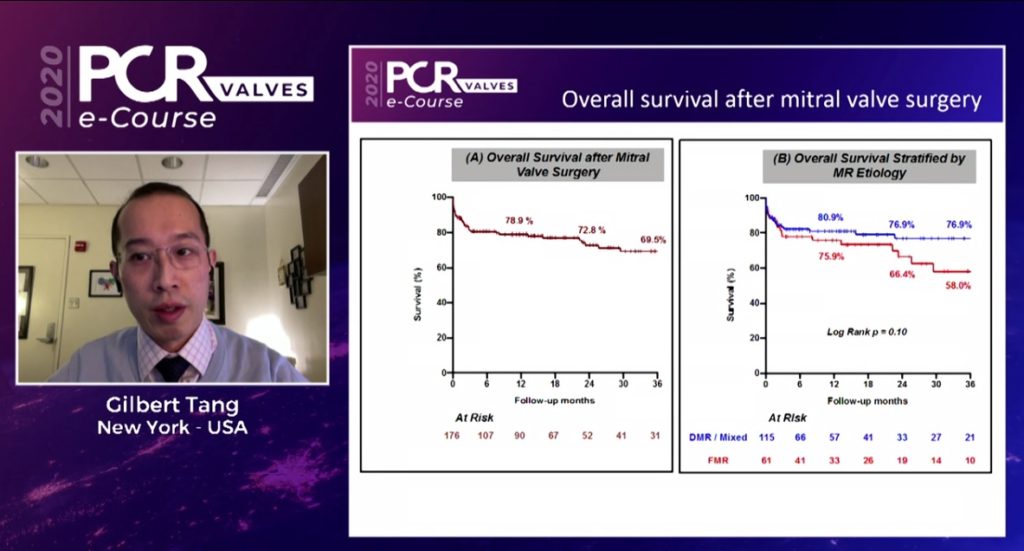
Functional mitral regurgitation patients had a shorter interval from transcatheter repair to surgery, Tang noted. He then showed Kaplan Maier curves for overall survival, showing that at around three years, survival is around 70%. Breaking this down into degenerative and functional mitral regurgitation, Tang commented that the data show 58% of functional mitral regurgitation patients worsening at three years versus 76.9% for DMR. Hospital length of stay was longer for patients with functional mitral regurgitation, 21 days compared to 16 days for those with degenerative disease.
Severe tricuspid regurgitation was the single most consistent predictor of 30-day and one-year mortality, Tang said, commenting: “This is interesting and is consistent whether it is pre-existing TR before the clip or after the clip, before the surgery or even after the surgery.”