John Ormiston, medical director and interventional cardiologist, Mercy Angiography, Mercy Hospital, Auckland, New Zealand, has investigated important innovations in interventional cardiology such as bioresorbable stents, TAVI and renal denervation. He told Cardiovascular News about these technologies, what drove him into cardiology, his career, and his hobbies, which include hiking in the wilderness in New Zealand.
How did you come to choose medicine as a career, and what drew you to interventional cardiology?
I was drawn to medicine because of the unique combination of science and its application to people. When I was a fellow, I heard Andreas Gruentzig speak at an American College of Cardiology meeting and was astonished. I thought that this could be an avenue to explore.
Subsequently Tony Roche, the cardiologist who introduced balloon angioplasty to Green Lane Hospital in Auckland, New Zealand, encouraged me to take part in the local programme that was in its infancy.
Who are the people who have influenced you the most?
My parents who knew the importance of education and hard work were a very strong influence. Sir Brian Barrett-Boyes, a charismatic internationally renowned, innovative insightful cardiac surgeon was an inspiration to many of us. He is legendary for contributions to homograft AVR, profound hypothermia and full repair of congenital heart disease in infancy. Peter Brandt, a cardiac radiologist, taught me his meticulous techniques for performance and analysis of coronary angiography. Tony Roche got me started in balloon angioplasty before his tragic death in a skiing accident. Barry Rutherford, a New Zealander based at the Mid America Heart Institute, Kansas City, is a wonderful teacher and has been like a father to me.
Which innovations in medicine shaped your career?
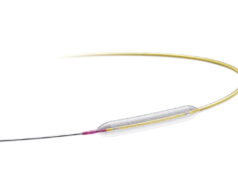
The innovations which shaped my career were balloon angioplasty, stenting, drug-eluting stents, resorbable scaffolds, transcatheter aortic valve implantation (TAVI), and renal denervation.
You have been involved with absorbable scaffolds from an early stage, became principal investigator of the ABSORB trials and implanted the world’s first fully bioabsorbable drug-eluting stent. Do you believe this technology is the way forward?
Bioresorbable scaffolds have great potential. Vasomotion is possible after partial resorption so that the vessel can change calibre in response to physiological stimuli. There is evidence that for an artery to be healthy it needs to be exposed to pulsatile and sheer forces. A metallic stent cages the artery and prevents the vessel being exposed to these normal forces.
In addition, the disappearance of foreign body removes the potential for ongoing inflammation. These factors may lead to more healthy vessels in the long term with for instance less neoatheroma and less late thrombosis.
Another difference from metallic drug-eluting stents is that a small amount of positive remodeling occurs and this potentially overcomes the “late catch-up” seen with metallic drug-eluting stents. Patients and cardiologists prefer a temporary scaffold rather than a permanent implant.
This is especially true in some parts of Asia. However, we still need to learn more about these scaffolds in, for instance, more complex disease, bifurcations, ostial lesions, and heavily calcified lesions.
What is your view of the results obtained with TAVI so far? Do you see any future in using the transcatheter approach in standard risk patients?
The results of TAVI in patients unsuitable for surgical aortic valve replacement are stunning. I think that it is likely that evidence will build for the transcatheter approach to be used in standard risk patients as technology improves (lower profile guide catheters) as we understand more about and learn to limit stroke, aortic regurgitation, and pacemaker need. This is all provided that valve durability is sustained.
You have bench tested many new interventional devices. How do you enjoy the process of verifying the correctness of a device?
I am fascinated by how devices work, how techniques work, what limitations a device may have, and the best ways to use them. It often surprises me that new techniques or devices are introduced with minimal bench testing. I like to use bench testing to explore clinical observations such as stent longitudinal distortion and to make clinical recommendations. Over the years, we have made a number of observations that have predicted device behavior in vivo and that have altered clinical practice. Some of these observations have been unpredicted. I enjoy using a wide range of imaging modalities to explore devices on the bench.
What is your opinion about renal denervation?
The results to date are very impressive and so far appear to be sustained over time. The reduction in blood pressure should translate into prolongation of life, to reduction of myocardial infarction and stroke. There are tantalising preliminary data on improvement in diabetes mellitus, heart failure, renal impairment and other problems. It is almost too good to be true but I think it is real. There are some very interesting new technologies in development.
What are you working on at the moment?
I continue our work on stent mechanical properties, and bifurcation techniques. We are working with engineers on novel ways to model flow and stresses in arteries and bifurcations and how changes influence these parameters. Clinically we are working on some very interesting resorbable drug-eluting scaffolds. Also we are working with a new renal denervation concept with very promising early results.
Which developing techniques and technologies are you watching closely for the future?
I am definitely watching renal denervation, TAVI and resorbable drug-eluting stents very closely.
What still fascinates you about interventional cardiology?
Above all I enjoy the clinical work, patient contact and making a difference to patients’ lives. Working with patients is very rewarding especially in interventional cardiology. I am fascinated by how devices work. I truly enjoy clinical trial work and we are fortunate to have excellent colleagues, study personnel and a relatively supportive environment so that we are involved in many first-in-human trials.
What are some of your proudest achievements?
I am proud of that work I have done which is original. I am also proud to have been involved with many first-in-human trials especially the Bioresorbable Vascular Scaffold (BVS) programme.
I am grateful and proud to have had the opportunity to play a major role in setting up and running Mercy Angiography, a private cardiac and peripheral facility. This organisation provides first rate patient care, research and has enhanced the professional lives of many colleagues. The institution has given me a lot of freedom and of control over resources. At Mercy Angiography we have introduced new technologies such as drug-eluting stents, TAVI and renal denervation well before the rest of the country, the region, and sometimes the world.
You volunteered as an English teacher in Fiji in 1966. Can you share that experience with us?
The villages I taught at were then accessible only by boat. The Pacific Island was beautiful with palm trees, white beaches, warm sea, fish and turtles. The pupils were delightful.
What are your interests outside of medicine?
I enjoy spending time with my family including my two adult “boys”. We like snow skiing and spending time at our beach house. I enjoy running every morning no matter what the weather with our dog, Betty, a Visla. We enjoy hiking in the wilderness and New Zealand has so many wonderful tracks. I also collect New Zealand art.
Fact File
Degrees, diplomas, fellowships, registration
1972 MB ChB, University of Otago
1975 Fellow, Royal Australasian College of Physicians, Cardiology Part 1
1978 Fellow, Royal Australasian College of Physicians, Cardiology Part 2
1979–80 National Heart Foundation of New Zealand Overseas Fellow
1986 Fellow, Royal Australian and New Zealand College of Radiologists
1987 New Zealand Medical Council Register of Specialists – Radiology
1989 New Zealand Medical Council Register of Specialists – Internal Medicine/Cardiology
2004 Associate Professor in Medicine, University of Auckland Medical School
2005 Fellow, Cardiac Society of Australian and New Zealand
2006 Emeritus Fellow Asian Pacific Society of Interventional Cardiology
2008 Fellow Royal College of Physicians, London
2009 Fellow American College of Cardiology
Experience and positions
1973–74 House surgeon, Wellington Hospital
1975 Registrar, North Canterbury Hospital Board
1976 Cardiology registrar, Wellington Hospital
19778 Cardiology registrar, Green Lane Hospital
1979–80 Research fellow, UCLA Department of Medicine (Cardiology), Wadsworth Hospital, Los Angeles, USA
1980–84 Registrar, Auckland Hospital Board
1985–present Interventional cardiologist, Cardiac Investigation Rooms, Green Lane Hospital, Epsom, Auckland, now called Auckland City Hospital
1990–present Medical director and interventional cardiologist, Mercy Angiography, Mercy Hospital, Epsom, Auckland. Partner Auckland Heart Group
2007–present Visiting interventional cardiologist, North Shore Hospital, Auckland
Society memberships
Cardiac Society of Australia and New Zealand, Auckland Medico Legal Society, New Zealand Medical Association, American Heart Association, Asia Pacific Society for Interventional Cardiology, New Zealand Interventional Cardiology Group, and European Bifurcation Club
International positions held
2003–2004 President Asia Pacific Society for Interventional Cardiology
200–present Honorary Board Member, Asia Pacific Society for Interventional Cardiology
2007–present Interventional Scientific Council of the American College of Cardiology, Transcatheter Therapeutics Board of Directors, EuroPCR Scientific Advisory Committee