A study—AIDA (Amsterdam investigator-initiated Absorb strategy all-comers trial)—presented at EuroPCR (16–19 May, Paris, France) and published in The New England Journal of Medicine has provided further evidence that the bioresorbable vascular scaffold (Absorb, Abbott Vascular) is associated with a higher rate of device thrombosis than is an everolimus-eluting, permanent metallic stent (Xience, also Abbott Vascular). However, it did not find evidence that implantation technique (eg. routine postdilation), or any other factor, was an independent predictor of scaffold thrombosis.
Previous studies of Absorb, such as the GHOST-EU registry and ABSORB II (three-year data), have indicated that the rate of device thrombosis may be higher with Absorb than it is with Xience. Furthermore, the two-year results of ABSORB III indicated that the rate of target lesion failure is higher with the scaffold. However, some in the interventional cardiology community have suggested that using an optimal implantation technique—known as “PSP”, which involves predilation, appropriate vessel sizing, and high-pressure dilation—may mitigate these apparent higher risks; both Abbott Vascular and the FDA recommend that this technique is used when implanting the scaffold.
The aim of AIDA was not to investigate the efficacy of this implantation technique; it was, as investigators Joanna Wykrzykowska (AMC Heartcenter, Academic Medical Center-University of Amsterdam, Amsterdam, The Netherlands) report in The New England Journal of Medicine, to “compare the bioresorbable vascular scaffold with the metallic stent in a patient population that reflects that seen in routine clinical practice”. However, the investigators were able to gather data for the scaffold being implanted with and without the PSP technique. “During the first year of enrolment, scaffolds were implanted according to the manufacturer’s instructions, which, at that time, did not include mandatory postdilation; postdilation was performed in 63% of the lesions in the scaffold group during the first year of enrolment. The steering committee recommended routine postdilation of the scaffold device from October 1 2014 onwards,” the authors report. Furthermore, a reference vessel diameter of <2.5mm (as estimated visually) was a key exclusion criterion—Absorb is not recommended for use in small vessels.
At two years, there was no significant difference in the rate of target vessel failure between patients randomised to receive Absorb (924) and those randomised to Xience (921). However, the rate of target-vessel myocardial infarction was higher with Absorb (5.5% vs. 3.2% for Xience; p=0.04) as was the rate of definite or probable device thrombosis (3.5% vs. 0.9%; p<0.001). Wykrzykowska et al comment: “The numbers of patients with definite or probable device thrombosis were higher in the scaffold group than in the stent group over all postimplantation periods (acute, subacute, and late).” They add: “Vessel size of 2.25mm or smaller, adequate device sizing, and postdilation were not associated with the occurrence of device thrombosis.”
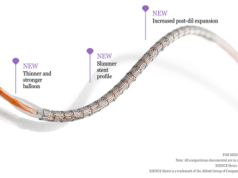
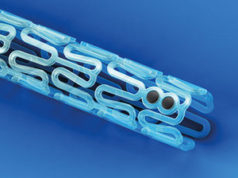
According to Wykrzykowska et al, the reasons for the higher rate of device thrombosis with Absorb are “only partly understood”. They note that incomplete lesion coverage, underdeployment, and malapposition “have all been observed with the use of optimal coherence tomography in acute and subacute cases of scaffold thrombosis”, and comment that the relatively thick struts of Absorb (150μm) may be associated with “blood-flow alterations and thrombogenicity, especially when they are left malapposed”. “Late events might be related to a combination of non-embedded and non-absorbed scaffold struts in complex lesions and late structures discontinuity or device dismantling,” the authors add, commenting that “the biology of the interaction between the device and vessel wall is very complex and so are the mechanisms of device failure such as scaffold thrombosis”.
Wykrzykowska et al state that their data and safety monitoring board recommended that they report their findings earlier than initially planned because of the increased incidence of very late scaffold thrombosis with Absorb. The board also recommended that the operators in the study should consider—on an individual basis—extending dual antiplatelet therapy (originally recommended for at least one year in both groups post procedure) in the patients who received a scaffold.
Prior to the trial, Abbott Vascular announced that Absorb would only available for use in clinical registries selected sites and institutions in Europe.
In response to the study, an Abbott Vascular spokesperson said: “The postdilatation pressures used in the AIDA study were below the current recommendation, and vessel sizing was not verified with imaging. Analyses of Absorb trials from around the world have demonstrated comparable results to Xience when implanted according to current instructions for use. We look forward to early results in the coming months of a more contemporary study (ABSORB IV) that is most reflective of current implantation techniques.”