Bjarne L Nørgaard (Department of Cardiology, Aarhus University Hospital, Aarhus, Denmark) and colleagues report in the Journal of the American College of Cardiology (JACC) that the use of computer-derived fractional flow reserve (FFRCT, HeartFlow Analysis, HeartFlow) in patients with intermediate stenosis—based on computed tomography (CT) angiography—is effective for differentiating patients who do not require further diagnostic testing or intervention from higher risk patients.
Coronary computed tomography (CT) angiography is increasingly used as the first-line test in patients with stable chest pain. It is excellent to rule out coronary artery disease, however, it overestimates stenosis severity and cannot assess flow over a stenosis which is the reference standard for decision-making in the cath lab, hence coronary CT angiogram is associated with excess use of downstream cath use. Therefore, new strategies are needed to identify those patients with coronary artery disease identified by CT angiogram, who may benefit from being referred to the cath lab and those who do not require further testing. Nørgaard et al has previously shown that FFRCT has “high and improved” diagnostic performance compared with anatomical interpretation with CT angiography alone, but they note “clinical outcome data in patients undergoing CT angiogram testing with FFRCT guidance are sparse”. Therefore, the purpose of the present study was to assess the clinical outcomes and safety using a diagnostic strategy including first-line coronary CT angiogram and selecting FFRCT in real-world patients with suspected stable coronary artery disease.
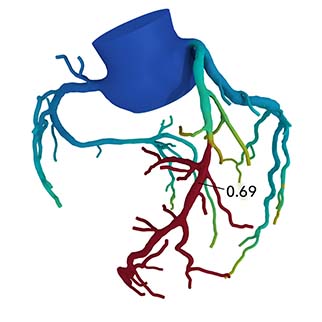
In the single-centre observational all-comer study, 3,674 symptomatic patients underwent CT angiogram on suspicion of stable coronary artery disease between 2014 and 2016. Of these, 697 patients with intermediate range stenosis (75% with stenosis >50%) underwent additional testing with FFRCT. “The 3D FFRCT model provides computed FFR values in all vessels of the coronary tree ≥1.8mm. The FFRCT result was negative when all values were >0.80 and positive when at least one value was ≤0.80,” the authors explain.
Of 677 (of 697 overall) with a conclusive FFRCT result, 61% had a value of >0.80 and 39% had a value of ≤0.80. Nørgaard et al comment that patients with values of ≤0.80 were more frequently treated with statins, antiplatelet agents, and beta-blockers six months after CT angiogram than were patients with values of >0.80. “Moreover, in patients with FFRCT ≤0.80, referral to invasive coronary angiogram was associated with higher statin and antiplatelet use when compared with those managed by planned optimal medical therapy alone,” the authors say.
The main finding of the study was that the rate of the primary endpoint—a composite of all-cause death, myocardial infarction, hospitalisation for unstable angina, and unplanned hospitalisation up to three years—was not significantly different between patients with <30% stenosis on CT angiogram and FFRCT values of >0.80 (both groups managed by optimal medical treatment and no further downstream testing). However, the risk of an adverse event was higher among patients with ≤0.80 who underwent invasive coronary angiogram and significantly higher in patients with values of ≤0.80 but did not undergo coronary angiogram (both groups received optimal medical therapy). Nørgaard et al say this higher risk was driven by a higher incidence of non-fatal myocardial infarction in the FFRCT values ≤0.80 and no invasive coronary angiogram.
The authors observe that their study “underscores the feasibility of selective FFRCT testing for decision making in patients with intermediate range coronary artery disease determined by first-line CT angiogram in day-to-day clinical practice”. They note that the findings extend those of the PLATFORM study—which showed that no major adverse cardiac events at 12 months occurred in 107 of 197 patients in whom invasive coronary angiogram was cancelled on the basis of coronary CT angiogram and FFRCT testing—because they confirm (in a large real-world practice cohort) that “deferral of invasive coronary angiogram in patients with intermediate-range stenosis, and a negative FFRCT result is safe even up to three years”.
“Further large-scale studies with longer follow-up are needed to further assess the risk and optimal management strategy in patients undergoing first-line coronary CT angiogram with selective FFRCT testing,” Nørgaard et al conclude.
Coinciding with its publication in JACC, the study was presented at the 2018 European Society of Cardiology (ESC) Congress (25–29 August, Munich, Germnay) by Bjarne L Nørgaard.











