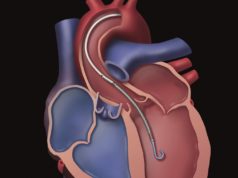
Mechanical circulatory support is frequently used to stabilise patient haemodynamics in desperate situations of circulatory failure to increase and maintain end organ perfusion.1 Of the available devices, the percutaneous micro-axial Impella (Abiomed) additionally provides a unique mechanism of left ventricular unloading.2 By reducing wall stress and increasing oxygen delivery, this might in itself be beneficial.3 In this commentary, Andreas Schäfer reviews the difficulties of evaluating the effectiveness of the system.
Cardiogenic shock represents a combination of patient conditions ranging from hypotension after acute myocardial infarction to out-of-hospital cardiac arrest often treated with multiple inotropes and/or mechanical circulatory support.1,4 It is challenging to differentiate patients in cardiogenic shock within the window of opportunity for treatment that might benefit from mechanical support from patients in the “haemo-metabolic state” who already have irreversible organ injury despite normalisation of haemodynamic parameters.5
Randomised trials play an important role in the assessment of therapies and innovative treatment options but present several logistic and methodological challenges.4,6,7 Therefore, evidence on the impact of mechanical support in cardiogenic shock based on randomised controlled trials is limited and currently mainly registry data and historical comparisons are available.7
Trial enrolment in cardiogenic shock
Given the low incidence rate of cardiogenic shock (approximately <10% of patients with acute myocardial infarction), slow enrolment has been observed in randomised trials with mechanical assist devices.4,6,8,9 Additionally, patients with cardiogenic shock have a high mortality and procedural risks, often due to the presence of multiple comorbidities and extensive coronary disease.2,7,10,11 Considering the emergent conditions in the setting of myocardial infarction and cardiogenic shock, obtaining consent from the patient is often impossible and seeking informed consent from the patient’s next of kin may cause additional delay.6,13 Also, the investigator-driven exclusion of study candidates that are expected to benefit from mechanical support may impact recruitment (selection bias).4 Last but not least it is important to conduct such randomised controlled trials in sites where experienced physicians and personnel are available 24/7 to make sure that mechanical support can be implanted at any time in optimal technical conditions.14
The exact definition of the targeted patient cohort by inclusion and exclusion criteria impacts both sample size and inclusion rate. A broad definition may increase the enrolment of patients in the trial but will also dilute the treatment effect and, thus, increase the sample size and potentially compromise identification of the beneficial effects of mechanical support. However, narrowing the inclusion criteria to exclude patients such as those with severe brain injury (e.g. following out of hospital cardiac arrest) may help to assess the impact of the targeted device but requires strict adherence to the protocol and severely reduces monthly inclusion rates. Appropriate definition of inclusion- and exclusion criteria, early identification of eligible patients, on-the-spot randomisation and subsequent enrolment in a trial with immediate initiation of support during an emergency situation presents a significant challenge.6
Outcome
Due to the life-threatening nature of cardiogenic shock and the known correlation of haemodynamic stability and maintained end organ perfusion with positive clinical outcomes, it is expected that mechanical support may affect the prognosis. Accordingly, the primary outcome of most randomised trials has been short- and long-term mortality. Overestimating the impact of primary haemodynamic stabilisation on mortality in cardiogenic shock can lead to false estimations when defining the potential effect size. Hence, calculating the sample size required to detect a significant difference in mortality probably contributes to underpowered study designs and thus inconclusive study results.15
Conclusion
The conduct of randomised controlled trials is an important element to scientifically understand emerging technical and therapeutic developments and verify their clinical relevance. As shown, the success of such studies depends on numerous aspects and requires dedicated compliance during execution. Running a trial with highly unstable patients in cardiogenic shock adds additional challenges from a logistic and ethical point of view. Using highly specific technology limits the number of specialized sites capable of conducting such trials.
Andreas Schäfer is at the Department of Cardiology and Angiology, Centre for Internal Medicine, Hannover Medical School, Hannover, Germany
References
- Rihal et al. J Am Coll Cardiol 2015; 65 (19): e7-e26.
- Basir et al. Am J Cardiol 2017; 119(6): 845–51.
- Basir et al. Catheter Cardiovasc Interv 2018; 91(3): 454–61.
- Thiele et al. Eur Heart J 2015; 36(20):1223–30.
- Kapur et al. AHA Scientific Sessions 2018.
- Ouweneel et al. Int J Cardiol 2016; 202: 894–96.
- van Diepen et al. Circulation 2017; 136(16): e232—68.
- Goldberg et al. Circulation 2009; 119(9): 1211–19.
- Sieweke et al. Eur Heart J Acute Cardiovasc Care 2018. Epub.
- Schwarz et al. Med Klin Intensivmed Notfmed 2016; 111(8):715–22.
- Harjola et al. Eur J Heart Fail 2015; 17(5): 501–09.
- Goldberg et al. Am J Cardiol 2004; 94(11): 1373–78.
- Dickert et al. BMJ 2015; 351: h3791.
- Henriques et al. Am Heart J 2014; 167(4): 472–79.
- Hochman et al. N Engl J Med 1999; 341(9): 625–34.