By Martin W Bergmann
Martin W Bergmann is an interventional cardiologist working in Germany, who performs percutaneous left atrial appendage (LAA) closure procedures. He explores why there is still a need for such procedures even in the era of novel oral anticoagulants and reviews the vital role of the interventional cardiologist in heart teams involved in LAA closure.
Novel oral anticoagulants are now used as first-line treatments to reduce the risk of stroke in patients with atrial fibrillation. They are seen as an attractive alternative to warfarin because they are associated with a reduced risk of intracranial bleeding and patients on these treatments, unlike those on warfarin, do not need have their INR levels closely monitored. However, they only reduce intracranial bleeding rather than eliminate it completely and there is still the possibility that patient may not adhere to treatment regimens (and therefore, be at increased risk for stroke).
Furthermore, how to treat patients who have experienced a stroke despite being on oral anticoagulation (secondary prevention), those who have had an intracranial bleed, those who have had a gastrointestinal bleed and those with an indication for intensified platelet inhibition after an acute coronary syndrome remains unclear. Therefore, additional options—aside from novel oral anticoagulants—for reducing the risk of stroke in patients with atrial fibrillation are still needed. As antiplatelet therapy is inefficient for stroke prevention, LAA closure is the only viable and effective alternative.
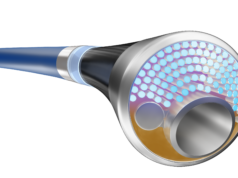
A large series of transesophageal echo studies prior to cardioversion, in patients with atrial fibrillation, found 90% of thrombi to be located in the LAA if no mitral stenosis was present, which prompted the development of devices and interventional techniques to occlude the LAA. The first randomised study in the field, which compared the Watchman single-disk LAA occluder (Boston Scientific) to warfarin treatment (PROTECT-AF), proved LAA closure to be non-inferior to warfarin therapy. The four-year follow up data of this trial (published in 2014) showed that Watchman device to be statistically superior to warfarin for reducing the relative risk of the composite primary endpoint of cardiovascular death, all stroke and systemic embolisation.
The US-based PROTECT-AF study found that periprocedural events to occur at around 5–10%. Growing experience and refinement of implantation techniques have improved safety of the procedure over the last years; this has been confirmed in the PREVAIL trial, which together with the PROTECT-AF data, led to FDA approval of the Watchman single-disk LAA closure techniques for all patients who are “not ideal candidates” for oral anticoagulation. Since 2012, European guidelines recommend that the device can be used in patients with relative or absolute contraindication for oral anticoagulation, which in practice is a very similar approach. Some countries like Germany have included LAA closure into their reimbursement for the above mentioned indication.
The decision to perform LAA closure should, ideally, involve a heart team consisting of an interventional cardiologist experienced in the procedure (>30 cases), the referring general practitioner or general cardiologist, and possibly also a neurologist. As the procedure requires experienced echo guiding to obtain good results, heart teams that are involved in performing structural heart interventions are particularly suited to planning and conducting the procedure.
With such a heart team in place, LAA closure with the Watchman device can now be performed with a periprocedural risk of around 1–2%.
Close collaboration between the referring physician and the interventionalist is also required to make decisions about the optimal post-implantation anticoagulation strategy. In Europe dual antiplatelet inhibition has become common standard after multicentre studies showed this approach to be safe; the randomised trials have been performed with a short 45-day course of oral anticoagulation with warfarin followed by dual antiplatelet therapy until six months after the procedure.
In summary, LAA closure has become part of routine care in patients with atrial fibrillation. New studies—such as the 1,000 patient, prospective Watchman LAA occlusion registry performed in Europe—have already completed enrolling and will shed further light on the role of this procedure. It appears probable that the number of patients in need of LAA closure will increase over the next few years; heart teams with experienced interventionalists are, therefore, needed to drive that development.
Martin W Bergmann,interventional cardiologist, Cardiologicum Hamburg, Hamburg, Germany