Multiple studies have shown that fractional flow reserve (FFR) is a valuable modality for assessing the functional significance of coronary lesions. However, it does have limitations—such as the need for a hyperaemic agent. Therefore, other modalities for physiological assessment have been developed to address this. This article, part of an educational supplement sponsored by Siemens Healthineers, explores the evidence behind these emerging cath lab tools.

Since it was first introduced in the cath lab in the 1990s, FFR has been established as a key tool for physiological assessment, and studies have shown that FFR-guided percutaneous coronary intervention (PCI) improves outcomes. Zimmermann et al, for example, performed an individual patient data meta-analysis of three randomised controlled trials of FFR.1 They found that “FFR-guided PCI [compared with medical therapy] resulted in a reduction of the composite of cardiac death or myocardial infarction compared with medical therapy, which was driven by a decreased risk of myocardial infarction.”
Furthermore, European guidelines give a Class I, Level of Evidence A recommendation (the strongest) for FFR, or an instantaneous wave-free ratio (iFR), to be used to assess the haemodynamic relevance of an intermediate-grade stenosis “when evidence of ischaemia is not available”.2
However, there are some challenges associated with using FFR and it may not always be the right tool. Joost Daemen (Department of Cardiology, Thoraxcenter, Erasmus Medical Center, Rotterdam, the Netherlands) points out that using a hyperaemic agent to “create an artificial stress test” in FFR can cause “some challenges”.
“Particularly in patients presenting with an acute coronary syndrome or in those with severe left ventricular hypertrophy, aortic stenosis, elevated left ventricular end diastolic pressures or mircovascular disease in which the interpretation of the obtained FFR value might not be straightforward. These patients may not respond predictably compared to those who do not have these issues,” he explains. He adds that the agent can also “cause symptoms that are quite uncomfortable for the patient at the point at which you administer it during your test … you might induce side-effects like dyspnoea or atrioventricular block. Also, the use of a hyperaemic agent adds time to the assessment, especially if you administer it through an intravenous catheter as that takes several minutes to deliver the agent.”
Physiological assessment without a hyperaemic agent
Given the issues associated with hyperaemic agents, several methods of performing physiological assessment without such agents have been developed. The most widely used of these is iFR, which, Daemen explains, is “based on a specific algorithm measuring the pressure gradient during diastole; a so-called wave-free period”. Thus, the need for a hyperaemic agent is negated. However, while iFR has been the “most widely tested” of the FFR alternatives, according to Daemen, it uses a patented algorithm of a single vendor. Several generic diastolic algorithms are now available, with Daemen noting “when assessed by multiple groups of researchers, these appear to correlate near perfectly to iFR”.
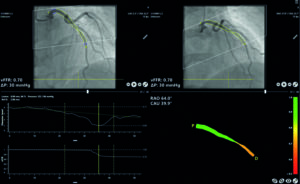
Another option is to remove the need for a pressure wire as well as for a hyperaemic agent. Angio-derived FFR measurement (3D angio-based FFR) uses angiogram data to compute FFR values. Daemen reports that it is a “relatively novel modality that is based on the fact that you can also model blood flow using computational fluid dynamics; that is a concept that has been applied to angio-based FFR.” As with wave-free period algorithms, several different modalities, such as CAAS vFFR (Pie Medical) sold by Siemens Healthineers, are available. He notes that vFFR has a “particular feature making it perhaps a bit easier to apply and faster because it uses the aortic blood pressure at the time of angio as an advanced condition to compute the flow”. Of note, Masdjed et al (including Daemen) evaluated vFFR in the FAST trial and found that “3D-QCA derived vFFR has a high linear correlation to invasively measured FFR, high diagnostic accuracy to detect FFR ≤0.80, and a low inter-observer variability”.3

Daemen does not believe that angio-based FFR modalities “will ever completely replace FFR”. But, he does think that they can potentially “drive the adoption of the physiological assessment”. “The total cases that use FFR [in some form] could significantly increase because performing physiological assessment—at potentially very low cost—will become a lot easier,” he adds.
Computed tomography (CT) can also be used to calculate FFR values (FFRCT). The PLATFORM study showed that FFRCT can be used to determine which patients with coronary artery disease require coronary angiography (and possibly revascularisation).4 Additionally, Hlatky et al report: “An evaluation strategy based on FFRCT was associated with less resource use and lower costs within 90 days than evaluation with invasive coronary angiography. Evaluation with FFRCT was associated with greater improvement in the quality of life than evaluation with usual non-invasive testing.”
Based on these findings, the main role of FFRCT in clinical practice is to rule out disease (and the need for invasive diagnostic tests); it is not a direct alternative to FFR as a patient may go on to have invasive testing (with angiography/FFR) if the modality indicates they have significant disease.
However, the SYNTAX REVOLUTION trial suggested that FFRCT could also be used to determine the optimal management approach for patients with coronary artery disease.5 Investigators Andreini et al state: “In patients with three-vessel coronary artery disease, a non-invasive physiology assessment using FFRCT changed the heart team’s treatment decision-making and procedural planning in one-fifth of the patients.”
Even if further trials support the findings of SYNTAX REVOLUTION, Daemen does not believe that this will signal the “end of the wire” (that is, invasive testing with angiography). “I do not think CT will replace angiograms. It has been shown to be perfect at ruling out disease. However, challenges with CT still remain in older patients with more calcified disease, previous stenting, bypass grafts, or those with kidney disease in which CT is less efficient. For these patients, who already have coronary artery disease, I am not so sure that non-invasive technologies will replace angiograms,” he says. For these patients, then, coming to the cath lab imaging-based assessment of physiological stenosis is the way of the future with the potential to be faster and reduce costs.










