According to the results of a large multicentre registry, patients who undergo transcatheter aortic valve implantation (TAVI) can suffer a rare and life-threatening complication—coronary obstruction. The registry, which was published in the Journal of the American College of Cardiology, investigated the main baseline, procedural characteristics and management of clinical outcomes in patients who experienced coronary obstruction.
Henrique B Riberio, Quebec Heart and Lung Institute, Laval University, Quebec City, Canada, and others, wrote that out of a total patients included in the registry (6,688), 44 patients suffered from coronary obstruction. Symptomatic coronary obstruction was secondary to the “displacement of the calcified native valve leaflets over the coronary ostia in the vast majority of cases”. Ribierio and colleagues also wrote that, although it incidence is reported (1%) in some TAVI studies, “data on this life-threatening complication have been limited to case report and very small case series.”
According to the results of the registry, baseline and procedural variables associated with coronary obstruction were older age (p<0.001), female gender (p<0.001), no prior coronary artery bypass surgery (p=0.045), the use of balloon-expandable valve (p=0.023) and prior surgical aortic bioprotheseis (p=0.045).
Although the incidence of coronary obstruction was said to be low for two types of TAVI systems (balloon expandable vs. self-expandable), coronary obstruction rate was twice as high in balloon-expandable valve (0.81%) than in self-expandable valve implantation (0.34%). Riberio et al explained that this may be because of differences in frame characteristics and the mechanisms for implantation, as well as differences in coronary height cut-off recommendations between manufacturers.
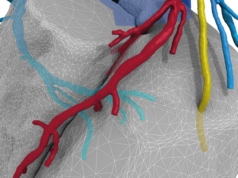
The authors also said that the left coronary artery was the most commonly involved and the mean left coronary artery ostia height and sinus of the Valsalva (SOV) diameters were lower in patients with obstruction compared to matched controls.
The majority of patients presented with persistent severe hypotension (68.2%) and ECG changes (56.8%). Riberio et al said that percutaneous coronary intervention (PCI) was attempted in 75% of cases with 81.8% being successful. They also noted in the study that 30-day mortality was 40.9% and after median follow-up (12 months) the cumulative mortality rate was 45.5% and there were no cases of stent thrombosis or reintervention.
Riberio and colleagues wrote that “the association between female sex and coronary obstruction may be due to anatomic differences in aortic SOV dimensions and coronary height according to sex”, therefore it occurs more frequently in women.
“Symptomatic coronary obstruction following TAVI was a rare but life-threatening complication […] despite successful treatment, acute and late mortality remained very high, highlighting the importance of anticipating and preventing the occurrence of this complication,” the authors said in conclusion.