 Vijay Kunadian (Newcastle University and Newcastle upon Tyne Hospital NHS Foundation Trust, Newcastle upon Tyne, UK) tells Cardiovascular News about her early career in interventional cardiology, the need for more concerted effort to improve outcomes among women with cardiovascular disease, and her research among elderly patients suffering from acute coronary syndromes.
Vijay Kunadian (Newcastle University and Newcastle upon Tyne Hospital NHS Foundation Trust, Newcastle upon Tyne, UK) tells Cardiovascular News about her early career in interventional cardiology, the need for more concerted effort to improve outcomes among women with cardiovascular disease, and her research among elderly patients suffering from acute coronary syndromes.
Why did you choose to become a doctor and why, in particular, did you choose to specialise in interventional cardiology?
I really loved science when I was in school, always coming top of the class, and at around 13 years of age I decided I wanted to be a doctor. Throughout medical school I absolutely loved everything about the heart—heart murmurs and structures really fascinated me—and wanted to be a cardiac surgeon. One of my first junior doctor jobs was in cardiothoracic surgery, but I did not enjoy that very much, so I switched gear. After medical training I took up post as a junior doctor in cardiology, and loved everything about it, particularly having great mentors who supported and encouraged me. My MD research project was all about coronary angiography and coronary artery blood flow, involving in-depth analysis of hundreds of coronary angios. I absolutely loved analysing the angios and I recall staying behind very late in the research office to make sure I was up-to-date with all my analysis. Then, as a clinical research fellow, I became interested in interventional cardiology. At the time we were not doing primary percutaneous coronary intervention (PCI) in the UK, but we were leading projects on rescue angioplasty. I was fascinated every time I was in the cath lab and I would always be welcomed by consultants and the cath lab staff that I did not feel any different as a woman in that environment. I was presenting work in nearly every cardiology congress, nationally and internationally, which sparked my enthusiasm for interventional cardiology. You could not get a consultant post in a tertiary cardiac centre in the UK at the time without an international overseas fellowship, and, as I was well ahead in my clinical training, I applied and was accepted to undertake an academic fellowship at Brigham and Women’s Hospital, Harvard Medical School (Boston, USA) which ignited my passion for academia.
Who were the biggest influences on your early career?
My dad has been the number one influence throughout my life, encouraging me to keep moving forwards, and break barriers. In my professional life, I am fortunate to have had great mentors from the early stages of my career. I learnt all about intervention and academia when I worked as a clinical research fellow under the supervision of Mark de Belder, and that is where it all started for me. I also had an absolutely incredible time in Boston as an academic research scholar with Mike Gibson. There was a very steep learning curve, but it was worth it. His attention to detail in everything—angiographic analysis, manuscript writing and reviewing, forward thinking—is so inspiring to me, and I still cherish everything I learn from him. I also got connected to Roxana Mehran as a Society for Cardiovascular Angiography & Interventions (SCAI) Women in Innovations (WIN) mentor. She is a truly remarkable person and an absolute honour to collaborate with. When such giants in interventional cardiology are supporting you, you really want to do the very best you can to provide outstanding care to patients through direct clinical care and research.
What has been the most important development in interventional cardiology during your career?
Having worked during the rescue PCI era, it is so amazing to see how primary PCI has transformed the way we deal with patients with ST-elevation myocardial infarction (STEMI). It is incredible to see the difference with lives being saved and very low complication rates. I was a trainee when we first performed transcatheter aortic valve implantation (TAVI) in Newcastle. That really was a memorable moment in my career. It is absolutely amazing how TAVI has evolved over the years and gives hope to patients who would normally have been turned down from open heart surgical procedures, particularly in the context of an ageing population with multi-morbidities.
What has been the biggest disappointment? Something you hoped would change practice but did not?
I am really so disappointed that we have not made much progress in the best care of women with cardiovascular disease. We have been talking about the fact that women are undertreated and have worse outcomes for decades, but have not really seen much change to improve outcomes. Even in 2022, papers are being published showing that women are undertreated for the various cardiovascular conditions leading to worse outcomes. The pandemic has not helped progress either, perhaps pushing the health and wellbeing of women backwards. This is why, as a commissioner on The Lancet Commission to reduce the global burden of heart disease in women by 2030, I am determined to see this mission realised through raising awareness and new clinical research projects. I was also chosen by the British Heart Foundation (BHF) as their panel member for the Bias and Biology campaign, and have campaigned on national media to improve the care of patients with heart disease, in particular women. I was an invited keynote speaker at the United Nations Commission on Status of Women event in 2021 discussing gender equality and equity in healthcare.
What are your current research priorities?
I have been leading on several research projects in Newcastle to improve the outcomes in older adults with acute coronary syndromes (ACS). Although 50% of myocardial infarctions (MIs) happen in over 70s, there is very sparse evidence on the best care of older adults. Hopefully our studies will help address the evidence gap in this cohort of patients.
What have recent studies taught us about treatment of elderly patients with ACS, and are there areas where research in this population is lacking?
In the last decade, there have been many drug and device studies which have increased the evidence base in older adults. For example, we can now safely give short duration dual antiplatelet therapy (DAPT) with latest generation drug-eluting stents for older patients without an increase in ischaemic events, but with reduced bleeding events. But, we still do not know if interventional strategies such as PCI or coronary artery bypass grafting (CABG) are of benefit equally in younger and older adults with ACS. We are studying this in the SENIOR RITA trial and hopefully we will have the results soon which will impact clinical practice worldwide. Although there is lack of evidence, it is also a challenge recruiting older patients to research studies.
What are the current challenges facing women seeking to enter the interventional cardiology field, and how would these be best overcome?
 Looking at the my own career, all of the barriers that women currently report have always existed, but it has not always been something I have taken to hamper my progress personally. I always sought out support and guidance from great leaders which helped refine and shape my career. I think the key for success is to shut out the negatives, keep seeking, and not to give up, because there are some remarkable leaders who would be willing to help and support you.
Looking at the my own career, all of the barriers that women currently report have always existed, but it has not always been something I have taken to hamper my progress personally. I always sought out support and guidance from great leaders which helped refine and shape my career. I think the key for success is to shut out the negatives, keep seeking, and not to give up, because there are some remarkable leaders who would be willing to help and support you.
In cardiology, and in medicine in general, there is no shortcut. Sometimes you might think ‘I am not going anywhere’, but these are times of growth and development. The bottom line is to make the most of opportunity and support from mentors, work hard, be proactive, always be willing to learn, be grateful, be respectful of others, and go with your passion. It is crucial that trainees are nurtured to strengthen the future workforce in our amazing specialty where there is much need for dedicated professionals.
Looking back over your career, what has been your most memorable case?
I have many memorable cases, but I always remember the history and story from female patients. The recurring theme is that women themselves, or their doctors, do not think they are having a heart attack, but in the end it is always the heart. I often present the case of a 50-plus woman who did not seek help for 12 hours. Her husband came home from work and saw her not looking well and then called for help. She was brought to the cath lab, where, en route, she had multiple cardiac arrests, was in cardiogenic shock, had a large thrombus in left main stem extending to the circumflex artery. When we aspirated the thrombus, there was no evidence of a lesion. But, an intravascular ultrasound (IVUS) showed plaque rupture in the ostium of the left main which needed to be fixed with stenting to save her life. You can see how we could have easily lost her if we did not undertake the right investigations and treatment.
Outside of medicine, what are your hobbies and interests?
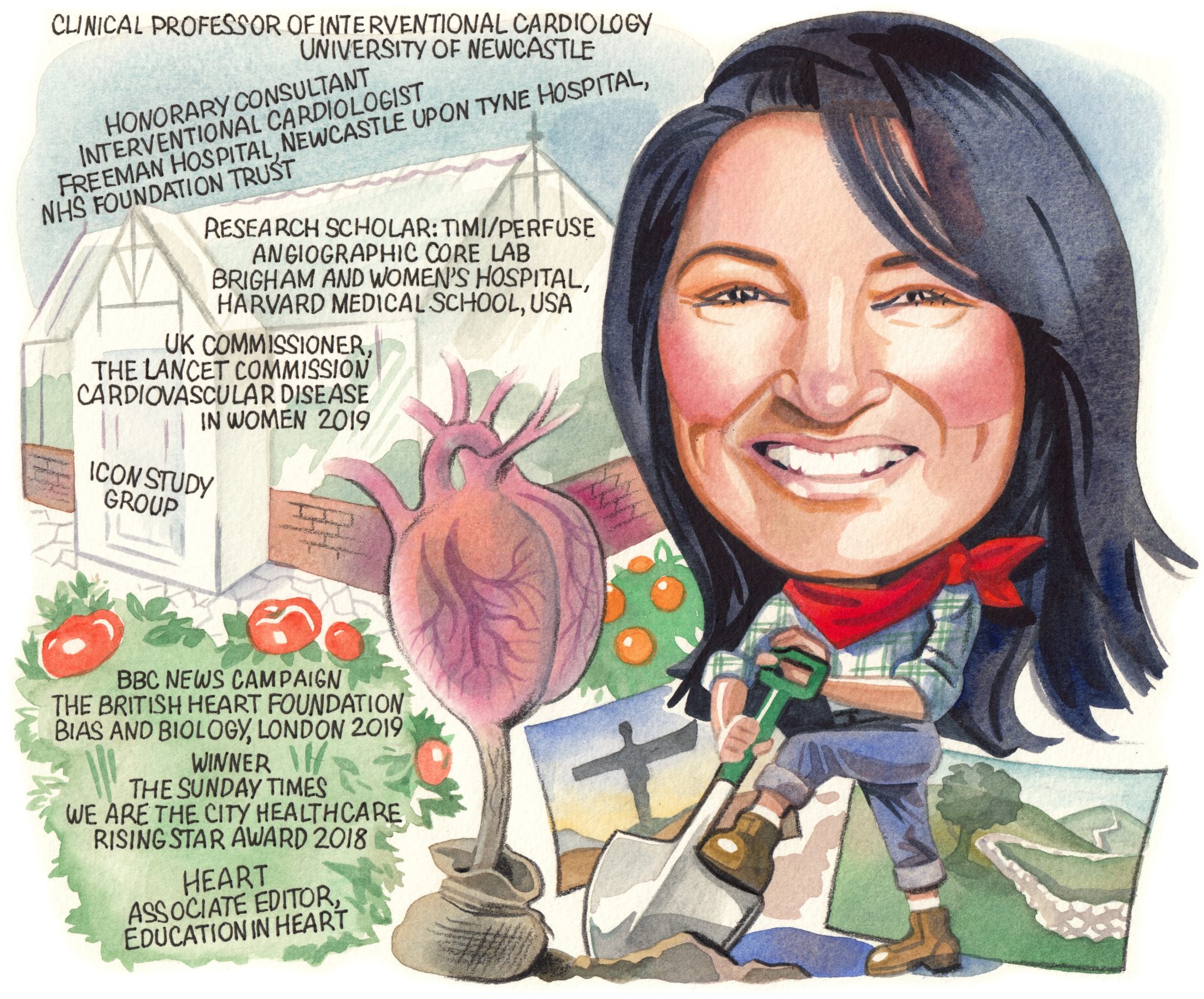
I have many interests and hobbies outside of medicine and cardiology. To name a few, I am a keen gardener, growing all sorts of flowers, fruits and vegetables in my garden. I love to cook and having family and friends around. I love hiking, and live in the stunning North East of England countryside and love long walks in the moors and up the hills. I love taking photographs of the stunning beautiful scenery during my walks.
FACT FILE
Current appointments
Personal Chair, Professor of Interventional Cardiology, Newcastle University
Honorary Consultant Interventional Cardiologist, Freeman Hospital, Newcastle upon Tyne Hospital NHS Foundation Trust
Lead Supervisor: MRes Cardiovascular Science, Newcastle University
Education & training
General and Interventional Cardiology, Northern Deanery, UK
Postgraduate Diploma in Clinical Trials, University of London, UK
Research Scholar, Brigham and Women’s Hospital, Harvard Medical School, USA
Research Registrar, The James Cook University Hospital, Middlesbrough, UK
Memberships
British Cardiovascular Society
British Cardiovascular Intervention Society
European Society of Cardiology
European Association of Percutaneous Cardiovascular Interventions
Royal College of Physicians
Editorial positions
European Heart Journal Digital Health, Associate Editor
Heart, Associate Editor, Education in Heart
Circulation Cardiovascular Interventions, Editorial Board













