New data for the PASCAL system (Edwards Lifesciences), which received the CE mark in February 2019 for the management of mitral regurgitation, suggest it may have a role in the management of tricuspid regurgitation. During the first-ever late-breaking trial session at TVT 2019 (12-15 June, Chicago, USA), Neil P Fam (Division of Cardiology, St. Michael’s Hospital, University of Toronto, Toronto, Canada) outlined a multicentre experience of compassionate use of the PASCAL system for patients with severe tricuspid regurgitation.
Fam reported that transcatheter leaflet repair of severe tricuspid regurgitation is a “promising treatment option for selected patients at prohibitive surgical risk”. However, he added: “Large tricuspid leaflet coaptation gaps and leaflet tethering represent common anatomical features that challenge the application of transcatheter repair techniques.”
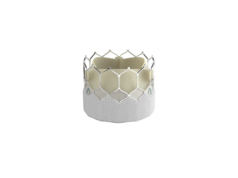
According to Fam, the PASCAL system has unique features that may enable it to over these anatomical challenges. These include a central spacer intended to the fill the regurgitation orifice area, broad contoured paddles to reduce stress on leaflets, and “clasps that allow for independent leaflet capture and the ability to fine tune leaflet position”. Additionally, he noted, “implantation elongation helps promote safe subvalvular manoeuvring”.
The aim of the present multicentre, observational compassionate use experience was to assess procedural and clinical results with the device for the management of patients with severe tricuspid regurgitation who—as determined by the heart team—were inoperable or high surgical risk. The key outcomes were the successful implantation of at least one device (post procedural tricuspid regurgitation grade ≤2+ with no mortality or conversion to surgery) and clinical and device outcomes at 30 days.
Of 28 patients in the intention-to-treat analysis, 24 (86%) underwent successful implantation with a mean of 1.4±0.6 devices implanted per patient and independent leaflet grasping achieved in 90% of patients. The average procedure time was 134±68 minutes and no patients died or were converted to surgery. By 30 days, two patients had died and one patient had been hospitalised for heart failure (despite sustained tricuspid regurgitation); however, there were no strokes, myocardial infarctions, conversions to surgery, or reinterventions.
Fam reported that, by 30 days, most patients had a significant reduction in tricuspid regurgitation (compared with baseline levels): 85% of patients had tricuspid regurgitation grade ≤2+ at 30 days. He observed that this reduction in tricuspid regurgitation was associated with a significant improvement in New York Heart Failure Association (NYHA) class—with 88% of patients in NYHA class I/II at 30 days. There was also, Fam said, a nearly 100m improvement in the six-minute walk test (on average).
He concluded that this first-in-human experience of the PASCAL system for tricuspid regurgitation indicated that the system was associated with “high procedural success, acceptable safety and significant clinical improvement in patients with challenging tricuspid anatomy and severe tricuspid regurgitation”. “Prospective studies with long-term follow-up are needed to confirm these initial promising results and further define the impact of the PASCAL repair system on clinical outcomes in patients with tricuspid regurgitation,” Fam added.