Over the last decade, the cath lab has transformed. Interventional cardiologists are now not only treating increasingly complex lesions, such as chronic total occlusions, but they are also treating increasingly complex patients (i.e. those that are older with more comorbidities). This article, part of an educational supplement sponsored by Siemens Healthineers, explores the challenges of today’s cath lab and how these can be addressed.

For Stephan Achenbach (Department of Cardiology, University of Erlangen, Erlangen, Germany), today’s cath lab has three key challenges. The first is that physicians are increasingly treating lesions that previously would have been treated by coronary artery bypass grafting (CABG). He says: “For example, we more frequently treat patients with chronic total occlusions compared with a few years ago when the likelihood was that those patients would be referred for CABG. So, anatomies that the interventionalist would not have touched a few years ago are now routinely being seen in the cath lab.”
The second challenge is that patients themselves have become more complex. They are older, which means that they are likely to have more comorbidities that require consideration. For instance, they may have reduced kidney function and, as a result, are less tolerant of contrast. For both of these challenges, Achenbach says, a good imaging system is vital.
He explains that complex lesions require “excellent image quality” so that the cath lab staff can properly visualise the lesion, and adds that the imaging system also needs to have good flexibility and angulation for the operator to properly access the target vessel. High image quality, Achenbach notes, is important when treating patients with reduced kidney function because it means they do not have to undergo imaging for a prolonged period. Therefore, less contrast is needed and the risk of acute kidney injury is reduced.
The third challenge facing the modern cath lab is that the goalposts have moved. Previously, according to Achenbach, getting the patient “off the table with a nice angiogram” was the only desired outcome. But, now, interventional cardiologists look at the long-term outcomes as well as the short-term outcomes. “These days, we know that we have to produce results that are at least as good as those of bypass surgery. So, we are not looking at the outcomes at one or two days after the procedure but five and 10 years down the line. This is something that is increasingly penetrating the consciousness of both general cardiologists and interventional cardiologists,” Achenbach observes.
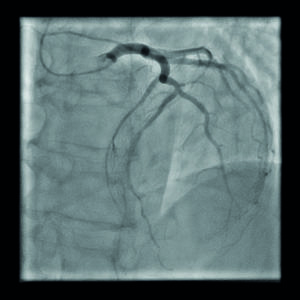
Furthermore, he says that studies have shown that percutaneous coronary intervention (PCI) can provide equivalent outcomes to surgery, as long as the optimal techniques are used. The SYNTAX II study, for instance, was a multicentre, all-comers, open-label study that compared a contemporary PCI strategy with the strategy used in the original SYNTAX study (SYNTAX I) to manage three-vessel disease.1 The contemporary strategy consisted of heart team decision-making using the SYNTAX Score II (combining anatomical and clinical factors), coronary physiology guided revascularisation, implantation of new-generation drug-eluting stents, intravascular ultrasound (IVUS)-guided stent implantation, and contemporary chronic total occlusion revascularisation techniques. In contrast, the previous strategy only used the original SYNTAX score (anatomical factors only) and PCI was performed with a first-generation drug-eluting stent.
At one year, the SYNTAX-II strategy was superior to the equipoise-derived SYNTAX I PCI cohort (p=0.006). This difference was driven by a significant reduction in myocardial infarction and revascularisation. Additionally, an exploratory short-term comparison with the equipoise-derived SYNTAX-I CABG cohort suggested that there were no significant differences in the rate of major adverse cardiac or cerebrovascular events at one year.
However, as indicated by SYNTAX II, multiple tools may be required to achieve optimal PCI outcomes: physiological assessment, such as fractional flow reserve (FFR), intravascular ultrasound (IVUS), and/ or optical coherence tomography (OCT). Achenbach notes that operators should not lose focus by becoming too wrapped up with these new technologies, stating: “It is important that we concentrate on the coronaries and are not distracted by the technology.”
Therefore, he believes that cath labs need a system that can integrate these modalities to make using them as “easy as possible”. Integration of information is particularly important because it helps operators make the right decision for patients. “A connected cath lab, for me, is one in which we can access all of the information we have about the patient. The data just have to be there.”
ARTIS icono
By reducing the complexity of cardiovascular procedures and supporting a smooth workflow, the ARTIS icono (Siemens Healthineers) is designed to address the challenges that Achenbach refers to.

It does this by providing the flexibility to access the patient from any side to support a wide variety of cardiac and vascular procedures, having fully motorised movements of the C-arm, providing automated, precise, and reproducible repositioning, and allowing quick and easy transition between imaging position and emergency case position. In particular, it has “Case Flows” that allow operators to standardise procedures for multiple ARTIS icono labs for more consistent documentation.
Another feature of the system is it has an ultra-low dose programme to reduce radiation exposure while delivering high-quality images. Achenbach says cath labs rely on systems that are designed to minimise radiation exposure because their procedures can be long and, thus, operators are potentially at risk of receiving high doses of radiation. “It has to be an essential and self-understood issue that radiation exposure is low. We need an intelligent solution to lower radiation exposure even in complex procedures without us even having to think about it,” he comments.
The ARTIS icono also has a “Third Party Broker” feature, which enables the next level in connectivity and communication and provides easy set-up for connection of different systems via a single connection, standard protocols, and a unified interface.
Achenbach uses the ARTIS icono at his centre and says he is “very happy” with the speed of the system because it means he has a smooth workflow.
References
- J Escaned, C Collet, N Ryan, et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. European Heart Journal 2017; 38: 3124–34.










