A trial of transcatheter mitral valve replacement (TMVR) with the Tendyne system (Abbott) led to successful treatment of severe mitral annular calcification (MAC) in nearly all patients, coupled with significant improvements in heart failure symptoms and quality-of-life parameters, prompting hopes of an effective treatment in a patient population currently with limited options.
These are findings of the SUMMIT-MAC trial, presented during a late-breaking trials session at the 2025 Transcatheter Cardiovascular Therapeutics (TCT) conference (25–28 October, San Francisco, USA) by Paul Sorajja (Abbott Northwestern Hospital, Minneapolis, USA), published simultaneously in the Journal of the American College of Cardiology (JACC).
MAC is a fibrous, degenerative calcification of the mitral valve support ring that is associated with mitral regurgitation (MR), stenosis, or a combination of these valvular lesions, and can pose challenges for surgical correction, limiting treatment options.
“We’ve known for a long time that safe options are needed for patients with severe MAC,” said Sorajja, noting that SUMMIT-MAC is the first non-randomised, prospective, multicentre clinical study to assess a dedicated TMVR system in this patient population.
Features of the device, which is retrievable and repositionable, include dual frame design, tether and apical pad. However, the need to deliver the device transapically is one potential drawback.
All patients enrolled in the trial had severe MAC, were considered high surgical risk and were approved by a case-review committee. An echocardiography core laboratory performed independent assessments of mitral disease for study inclusion and assessed all follow-up echocardiograms.
A total of 103 patients with severe MAC and mitral valve disease (either mitral regurgitation or stenosis) underwent an attempted procedure with this transcatheter mitral valve system at 37 centres in the USA.
The trial’s population was described as elderly (78±6.5 years), with nearly half aged 80 years or older, and the majority were women (57%). Significant comorbidities, including atherosclerosis, renal disease, chronic lung disease, and pulmonary hypertension, were common.
Most patients (97.1%) had MR grade 3+ or 4+ at baseline, and severe mitral stenosis (MS) was present in 12 patients (11.7%). Baseline mitral gradient in these patients was 5.3±2.2 mmHg. The average MAC volume for the SUMMIT-MAC cohort was 5,679±5,670mm3, with 46% of patients expected to have some encroachment of the valve frame due to the configuration of the MAC. However, the device was successfully implanted in all cases, Sorajja reported.
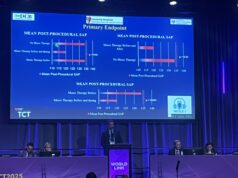
The primary endpoint of freedom from all-cause mortality and heart failure hospitalisation at one year was met, and one-year freedom from all-cause mortality and freedom from heart failure hospitalisation rates were 79% and 69.9%, respectively. Bleeding was the most common severe adverse event with apical access site bleeding occurring in 5.8% of patients.

At one year, 97% of patients had mild or no mitral valve regurgitation. In addition, heart failure symptoms improved significantly with only 13% of patients having New York Heart Association (NYHA) class III symptoms compared with 73% prior to the procedure. Quality of life also improved at one year with an average 18.7-point increase in the Kansas City Cardiomyopathy Questionnaire (KCCQ) score.
“These patients actually don’t have a good option,” said Sorajja, summing up the results of the trial and speculating on whether the results could prompt a change in guidelines for the treatment of MAC. “These are patients who were not qualified for surgery and not qualified for any available transcatheter option.
“What we showed in this trial is for a group of patients that had no options, we finally have an option that met the study endpoint and was meaningful in terms of clinical benefit. So, I do believe that this will change the clinical guidelines.”
Sorajja was quizzed on whether there may be alternatives to the transapical delivery, which he commented may warrant careful heart team consideration when deciding which patients to treat.
“The total apical or thoracotomy fatality rate was 2.9%. So, about a 3% risk of dying from this wound. Can we pick patients that may be a lot less risk; somebody who’s not on steroids, somebody who has good chest cavities, somebody who’s younger? Probably. I think with surgical experience, in the setting of left ventricular (LV) dysfunction, there’s an experience factor for that. So, I think it’s a heart team discussion.”