Cutting balloon angioplasty and the use of a super-high-pressure non-compliant balloon have been shown to be non-inferior to intravascular lithotripsy (IVL) in separate randomised trials comparing the calcium modification techniques to IVL.
These are the findings of two trials presented during a late-breaking trials session at the 2025 Transcatheter Cardiovascular Therapeutics (TCT) conference (25–28 October, San Francisco, USA)—ShortCUT and VICTORY—which examined strategies for preparing calcified coronary lesions prior to PCI.
“There are multiple device options available for calcium modification, however, there are limited direct comparisons between these devices, many of which have different mechanisms of action and carry substantial differences in cost,” commented Suzanne Baron (Baim Institute for Clinical Research, Boston, USA), an investigator in the ShortCUT trial, which directly compared the safety and efficacy of cutting balloon angioplasty to IVL prior to drug-eluting stent (DES) implantation in over 400 patients.
The trial enrolled 413 patients with stable or unstable coronary artery disease with de novo calcified coronary lesions at 21 sites in the USA and was stratified to include two separate cohorts of patients: those with planned up-front rotational atherectomy (n=208) and those in whom up-front rotational atherectomy was not planned (n=205). In each cohort, patients were randomised to receive IVL- or cutting balloon-facilitated lesion preparation.
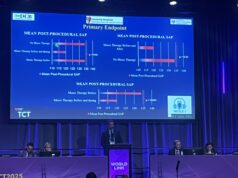
ShortCUT’s primary endpoint was post-procedural stent area at the site of maximal calcification as measured by core lab-adjudicated, high-definition intravascular ultrasound assessment.
The study found that for the post-procedural minimal stent area (MSA), the mean was 8.6 mm2±2.5 for IVL and 8mm2±2.4 for the cutting balloon strategy. Baron detailed that, when the primary endpoint was stratified by atherectomy plan, results were similar to the overall study cohort in those patients who underwent planned atherectomy but in patients who did not undergo planned atherectomy, cutting balloon angioplasty did not meet non-inferiority. “This may have been partly due to differences in vessel size between groups, as stent expansion and indices of calcium fracture were similar,” she said.
Average stent expansion at the site of maximum calcification was similar with 97.7±24 for IVL and 97.7±25.9 for the cutting balloon. The procedural cost difference was US$3,632 with the main cost difference being driven by the cost of the randomised device.
Strategy success, defined as stent delivery with a residual stenosis less than 20% in the absence of significant angiographic complication and not having to use alternative calcium modification devices, was also similar with 89.7% for IVL compared with 89.2% for the cutting balloon. Thirty-day major adverse cardiovascular and cerebrovascular event (MACCE) outcomes were the same between groups at 2.9%.
“Cutting balloon angioplasty is a reasonable and less costly option when compared with intravascular lithotripsy for the treatment of significantly calcified coronary lesions treated with imaging guided PCI,” Baron concluded.
VICTORY, meanwhile, compared IVL to the OPN NC balloon (SIS Medical), a super-high-pressure coronary balloon, for lesion preparation. The primary endpoint of the trial was final stent expansion assessed by optical coherence tomography (OCT) determined by an independent imaging core laboratory.
Matthias Bossard (Luzerner Kantonsspital Heart Center, Lucerne, Switzerland) detailed that a total of 282 patients at three sites in Switzerland and Canada were randomised one to one to IVL (n=142) or the super-high-pressure balloon (n=140).
The balloon group achieved a median of 85% stent expansion compared with 84% in the IVL group, meeting non-inferiority. The use of the balloon resulted in similar rates of acute procedural (98.6% versus 97.1%) and strategy success (98.6% for both) compared with IVL. The results were consistent across a number of patient subgroups. In addition, there were no significant differences in safety outcomes including coronary artery dissections, perforations, or side branch occlusions.
“We think we know now that the OPN is non-inferior to IVL in terms of stent expansion,” Bossard said of the results. “VICTORY indicates that OPN and IVL have a similar safety profile. The OPN potentially represents a reasonable lower cost alternative to IVL, which may be faster to use.”
Commenting on the data during a TCT press conference, Azeem Latib (Montefiore Medical Center, New York, USA), said that the two studies were indicative of IVL’s status as a standard of care treatment for calcified coronary artery disease, in large part due to the ease of the technique.
“Everybody sees IVL now as the standard of care in calcified lesions because it has democratised treating calcified lesions,” he said. “Before, it was pretty difficult, smaller centres were not able to do it, now they have this very safe technology, but it costs a lot of money, and so other technologies that are less expensive are trying to compare themselves against the standard of care.”