 Lesion selection for percutaneous coronary intervention (PCI) using the non-invasively assessed physiologic measurement quantitative flow ratio (QFR) improved outcomes for PCI compared with a standard angiography-guided strategy, investigators in the FAVOR III China trial have found.
Lesion selection for percutaneous coronary intervention (PCI) using the non-invasively assessed physiologic measurement quantitative flow ratio (QFR) improved outcomes for PCI compared with a standard angiography-guided strategy, investigators in the FAVOR III China trial have found.
Findings of the trial were reported during a late-breaking trial session at the Transcatheter Cardiovascular Therapeutics annual meeting (TCT 2021, 4–6 November, Orlando USA and virtual) and simultaneously published in The Lancet. Investigator Bo Xu, director, Catheterization Laboratories at Fuwai Hospital in Beijing, China commented that the simplicity and safety of QFR compared with wire-based physiological measurements, should facilitate its adoption in routine practice.
QFR, derived from three-dimensional coronary artery reconstruction and fluid dynamics computations from the angiogram, enables online estimation of fractional flow reserve (FFR) without the use of a pressure wire or pharmacological agents to induce hyperaemia.
Prior studies have demonstrated the feasibility and accuracy of online QFR assessment in assessing the haemodynamic significance of coronary stenoses compared with pressure wire-based FFR measurement. FAVOR III China was an investigator-initiated, multicentre, blinded, randomised, sham-controlled trial that compared QFR and angiography for lesion selection and monitored outcomes for one-year post procedure.
Patients with stable or unstable angina pectoris or those more than 72 hours post-myocardial infarction who had at least one lesion with a diameter stenosis between 50% and 90% in a coronary artery with a reference vessel diameter of at least 2.5mm by visual assessment were randomised 1:1 to a QFR-guided strategy (PCI performed only if QFR ≤0.80) or an angiography-guided strategy (PCI based on standard visual angiographic assessment).
Between December 2018 and January 2020, 3,825 participants at 26 sites were randomly assigned to QFR-guided PCI (n=1,913) or angiography-guided PCI (n=1,912). The mean age was 62.7 years, 70.6% were men, 33.9% had diabetes, 63.5% presented with an acute coronary syndrome, and 54.0% had multivessel diseases. All patients, post-cath lab physicians, and research personnel were blinded to treatment allocation.
Participants in both arms underwent a preset 10-minute delay for real or sham QFR calculation before PCI. The target vessels intended to be treated with standard angiography guidance were declared by operators and recorded prior to randomisation.
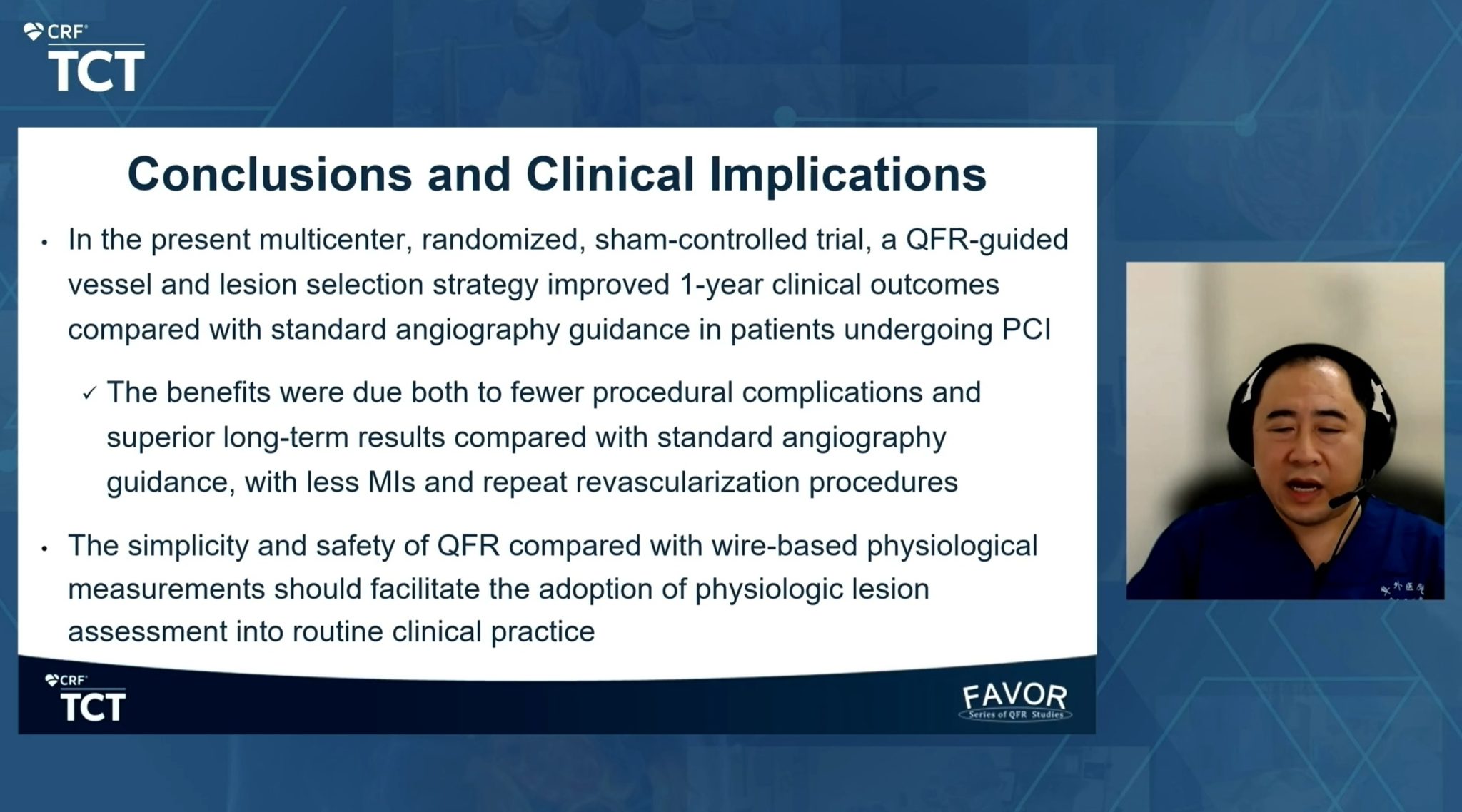
The primary endpoint of the one-year rate of major adverse cardiac events (MACE), a composite of death from any cause, myocardial infarction, or ischemia-driven revascularization, was 5.8% for the QFR guided group compared to 8.8% for the angiography-guided PCI group (HR 0.65, 95% CI: 0.51-0.83, p=0.0004). The major secondary endpoint (one-year rate of MACE, excluding peri-procedural myocardial infarction) was 3.1% for the QFR-guided group versus 4.8% for the angiography-guided group (HR 0.64, 95% CI: 0.46-0.89, p=0.0073).
“A QFR-guided vessel and lesion selection strategy improved one-year clinical outcomes compared with standard angiography guidance in patients undergoing PCI, due both to fewer procedural complications and superior long-term results.” said Bo Xu, MBBS, Director, Catheterization Laboratories at Fuwai Hospital in Beijing, China. “The simplicity and safety of QFR compared with wire-based physiological measurements should facilitate the adoption of physiological lesion assessment into routine clinical practice.”
Findings of FAVOR III could greatly expand the use of physiology in patients undergoing PCI, according to Gregg W Stone (Icahn School of Medicine, Mount Sinai, New York, USA), who was an investigator on the trial.
“For the first time we have clinical validation that lesion selection with this method improves outcomes for patients with coronary artery disease undergoing stent treatment,” Stone commented, following the presentation of the trial’s results. “By avoiding the time, complications, and extra resources required to measure lesion severity using a pressure wire, this simpler technique should serve to greatly expand the use of physiology in patients undergoing cardiac catheterization procedures.”
Stone further commented that he would expect to side wide adoption of QFR assessment as a result of these findings. “The results from this large-scale blinded randomised trial are clinically meaningful, and similar to what would have been expected with pressure wire-based PCI guidance. Based on these findings, following regulatory approval I would anticipate QFR to be widely adopted by interventional cardiologists to improve outcomes for their patients.”