Data from the MITRAL (Mitral Implantation of Transcatheter valves) study indicate that transeptal transcatheter mitral valve implantation (TMVI), with a Sapien 3 device (Edwards Lifesciences), may be a reasonable approach for high-risk patients with a failing surgical mitral ring.
MITRAL reviewed the outcomes of TMVI with the use of balloon- expandable aortic transcatheter heart valves to treat mitral valve disease in three patient cohorts: those with calcified native valves (mitral annular calcification arm); those with a failing surgical mitral ring (valve-in-ring arm), and those with a failing surgical mitral valve (valve-in-valve arm). There were 30 patients in each cohort; the primary safety endpoints were technical success at exit from cath lab and procedural success at 30 days, the primary effectiveness endpoint was patient success at 1 year and the secondary safety and effectiveness endpoint was a composite of various adverse effects at 30 days and one year.
The mitral annular calcification and valve-in-ring data were presented at the 2017 Transcatheter Cardiovascular Therapeutics (TCT) meeting (November 1st, Denver, USA) while the valve-in-valve data were presented at the 2017 American Heart Association (AHA) scientific sessions (November 13th, Anaheim, USA). Cardiovascular News spoke to Mayra Guerrero (Division of Cardiology, Evanston Hospital, Evanston, USA), who presented the data both at TCT and at the AHA, about the study.
How many patients with a surgical mitral ring or a surgical mitral valve are likely to require secondary intervention?
Studies show that at least 30–35% will require repeat surgery within 10 years.
Why might such patients require a percutaneous secondary intervention?
A percutaneous intervention provides a less invasive option at lower risk for the patient.
What is the rationale for using a TAVI device to treat patients with mitral valve disease?
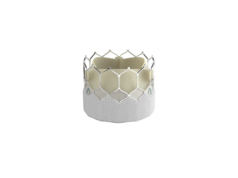
Balloon-expandable valves, such as the Sapien 3 device, fit well within most prosthetic valves in a mitral (or any) position. They are also suitable for some mitral surgical rings and for some patients with severe circumferential mitral annular calcification. Additionally, the Sapien 3 valve is commercially available and operators are familiar with it; therefore, it could be used for this purpose in carefully selected patients.
What were the key findings of your study?
In the valve-in-valve arm, all patients were treated with trans-septal access. There was no in-hospital mortality and no cardiac death at 30 days. There was one non-cardiac death at day 29 after the procedure and this was related to the patient choking on pills at home (3.3% 30 day all-cause mortality).
For the valve-in-ring arm, both all-cause in-hospital and 30-day mortality (6.6%) were lower than seen with valve-in-ring in the TVT Registry (9.3% and 13% respectively).
For patients with mitral annular calcification, all-cause in-hospital (16.7%) and 30-day (17.2%) mortality were lower than that seen in the TMVI in MAC global registry (23.3% and 25%). However, work is needed to refine techniques and patient selection to continue to improve outcomes.
In the valve-in-ring arm, 20% needed a second valve during the implantation procedure. Why do you think this was?
From this experience, we have learnt that the transcatheter valve needs to be implanted in a more ventricular position aiming 80% ventricular and 20% atrial. When it is too atrial, there may be paravalvular leak if the inner skirt does not cover the annulus. Therefore, the need for a second valve can be avoided with an improved implantation technique. We also think that, perhaps in the future, minor modifications to the valve—such as a longer inner skirt—may reduce the risk of needing a second valve.
What further studies are needed in this area?
We need to explore the role of valve-in-ring for patients at intermediate risk. We also need to conduct more studies of TMVI options in high-risk patients with mitral annular calcification.