Born in India and raised in Pittsburgh, USA, Susheel Kodali now practices in New York, where he is the director of the Structural Heart & Valve Center at NewYork-Presbyterian and the Avanessians associate professor in medicine at Columbia University Irving Medical Center. Specialising in structural heart disease, Kodali has been a key figure in the PARTNER trial, the world’s first prospective, randomised trial for transcatheter aortic valve implantation (TAVI), as well as being at the forefront of research into transcatheter tricuspid valve intervention. In this interview, Kodali discusses his early career, influences and latest research.
This profile features in issue 64 of Cardiovascular News.
What influenced you to pursue a career in medicine, and why did you choose to specialise in interventional cardiology in particular?
My parents and a couple of other family members were physicians, and what you get exposed to, is what drives a lot of your interests. But that being said, I went to Stanford University as an undergraduate, and started there as a computer science major. This might have been a better career path because in my class there were a lot of founders of large tech companies!
I enjoy things that involve logical paths from step A to step B, and I saw computer sciences as involving action and reaction. This goes into why I went into interventional cardiology as well. It is the technical aspects of it as well as the pace of innovation and change. During medical school I went through a lot of different paths. Initially, I was interested in neuroscience and neurology, but I eventually settled on pursuing either critical care or cardiology. A lot of my interest was driven by the technical aspects of the two fields. Both of them deal with acutely ill patients where an intervention is performed and immediately a clinical change is seen. In the end, the reason I went down the interventional cardiology route was the rapid pace of innovation.
Who have been the major influences throughout your career?
Clearly, one person stands out: Marty Leon. I always tell fellows, sometimes in terms of your career it is just a case of being in the right place at the right time, and when opportunities present themselves you take advantage.
I did all of my training out in California. I did my medicine, cardiology training at University of California, San Francisco (UCSF) and I decided to get a different experience for my interventional cardiology fellowship, and came out to New York. My wife and I had planned to be in New York for a year and then go back to California.
I came to Columbia before Marty Leon, Jeff Moses, and the entire group moved here. I started in July and they moved in the August. I was the only fellow here and so I got to work very closely with Jeff Moses and Marty Leon. Marty then asked if I was interested in staying on for another year because the REVIVAL trial, which was the first early feasibility study of transcatheter valve replacement, was starting at Columbia, one of the three sites in the USA.
Marty Leon has been the single most important mentor in helping my career move forward. He is a visionary, but he also provides other people opportunities. It is an incredible skill and an incredible strength of his. He recognises when people are deserving of opportunities and he will mentor them and help them to advance. I can definitely say I am where I am now because of Marty’s support. I consider myself incredibly lucky to have had the opportunity to work with him. I am one of many in field who he has helped develop.
During your career in interventional cardiology, has there been any one development that you think has shaped the field more than any other?
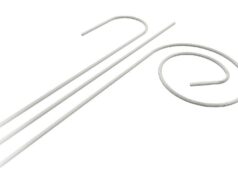
I do not think anything else compares to TAVI. It is such a disruptive, revolutionary technology that has changed the way we practice medicine and has opened up treatment options to patients that were not getting treated. It is something that clearly improves survival, improves quality of life, and it is a complete mind shift in how we address this disease. It has changed guidelines, repeatedly, and they still cannot keep up because of all of the data that that is coming forward.
I had the fortune to be in the TAVI space early, first in 2005, and it has really evolved and iterated over the next 15 years to a much more predictable, reliable procedure. But that did not come easy, that came because people looked at it rigorously. The majority of publications from the PARTNER trial onward are about the impact of complications on outcomes, looking at stroke and its impact, looking at vascular complications, looking at bleeding, and looking at paravalvular leak (PVL). Those are what drove innovation in the field—devices got smaller and there were solutions for PVL. There needs to be further innovation.
Is there anything that has had potential to change practice, but has not done so?
At this point I expected to have more options for treating mitral valve disease, and though it is not a failure of devices, I do think it speaks to the complexity and the variability of the disease process. Whether or how we will get there and what the options will be for mitral disease, are still a way off. I think perhaps it was underestimated how difficult it was going to be.
On the TAVI side, I think there are still opportunities for innovation. We can look at this and see what the weaknesses are, whether it is bicuspid valves, whether it is small annuli, and how we understand who is better with what and continue to iterate. Continuing to find ways to reduce complications is important.
What are your current research interests?
Clinically, TAVI and trials with new generation devices we are still very involved in. But, what has really been driving most of my time and energy has been looking at transcatheter options for treating tricuspid regurgitation. We have been involved in this space for more than five years and we have continued to work with the different technologies. I think the space is incredibly exciting.
Part of the challenge in tricuspid valve disease is in terms of the guidelines. We do not know, unlike with aortic and mitral valves, when we should treat these patients.
A lot of the initial learnings are going to be when and who we should we treat, in addition to understanding how these novel devices work. In certain patients, in certain disease morphologies and at certain stages, certain devices may work more than others. Unfortunately, many of the patients we are still seeing right now are a little too late in the disease process. So we need to understand how much benefit they are going to get versus whether we should we be treating these patients earlier upstream.
 What do you feel are the important questions that future TAVI trials need to address?
What do you feel are the important questions that future TAVI trials need to address?
We need better understanding of one device versus another device. But, I think an important issue we need to address is the lifetime management question. We are treating younger patients now, so if you do a TAVI in someone at 65 and the average survival is another 20 plus years, are they going to be able to get through their life without surgery? And that is an important part of the conversation with patients.
Durability issues are critical to understand, as is the ability to do valve-in-valve and what kind of results you are likely to get with these procedure. These are important questions that we need to answer for all the different devices.
Another important question is with bicuspid valves. We have some data, but it is limited and in selected patients who were felt to be anatomically suitable for TAVI in a bicuspid valve.
I do not know that we will need dedicated TAVI devices for bicuspid, my personal feeling is we need leaflet modification technologies to allow the current TAVI devices to work in the bicuspid valves, because the real problem is valve expansion. Whether it is lithotripsy to soften the calcium, leaflet laceration to allow complete expansion, or other technologies that modify the leaflets to allow TAVI to work in these bicuspids, I think that is where we need to go.
What do you think is likely to be the biggest talking point in interventional cardiology in the year to come?
It is not my area of expertise, but if you look at percutaneous coronary intervention (PCI) versus coronary artery bypass grafting (CABG) with the fractional flow reserve (FFR) trial published last year, that has generated a lot of discussion. There are arguments that say you could look at the data and look at the population enrolled to say it completely changes our practice, or to say this is this is a starting point and we need to learn more. But, I think that debate is never going to go away and the conversations seem to have ramped up in this past year.
You are a founder of the Fraternity of Advanced Cardiovascular Techniques and Solutions (FACTS). What are you proudest of about your work with the organisation?
It is heavily driven by my colleague in India, Sreenivas Kumar. I have an Indian background, having been born there, and despite growing up in the USA we would go back often. It was important to me to be engaged and, when I had the opportunity, to work with colleagues there on educational aspects of interventional cardiology. It was very exciting.
I am fascinated by the level of enthusiasm and how people are excited to talk about trials and next steps, and to learn and grow. As a result of the partnership between FACTS and through Marty Leon and the Cardiovascular Research Foundation (CRF) we are able to bring a lot of educational programmes to India with people like Marty, Eberhard Grube and others to be a part of the community there. Interventional cardiology is not just a western world specialty—it is a broader community. It is really exciting for me to be a part of that, the conferences that have grown out of it, the connections I have made with other people there.
Looking back over your career, are there any cases in particular that stand out to you?
There are a lot of them! There was a patient just a month ago who came into the cath lab, and he arrested due to a thrombus in the left main. We did CPR, put him on ECMO and opened the artery. Then, from thinking he was not going to survive, he managed to go home and leave the hospital. There are a lot of times that you see cases like that which are remarkable.
More so than that, I would say many of the patients that I have met are remarkable themselves. There are just a lot of stories. Because the space I work—transcatheter valve—has an elderly population, there are a lot of people of that generation to have served in World War Two. I have done procedures on patients that were Holocaust survivors, or were injured in the Battle of the Bulge. Hearing these remarkable stories and getting a chance to meet these people is one of the most rewarding aspects of the job.
Outside of medicine, what are your hobbies, interests and passions?
I have three boys in the 11th, ninth and fifth grade, they keep my wife and I occupied! Although I do not play a lot of sport I enjoy watching sport with my kids. American football is my main passion, and I am a big Pittsburgh Steelers fan. The season starts in August and ends in February, so for that period of time it is my main interest. I also love to travel, that keeps me going.
Fact File
Appointments
Columbia University Irving Medical Center, Avanessians Associate Professor of Cardiology
Fraternity of Advanced Cardiovascular Techniques and Solutions (FACTS), co-founder
Education
Stanford University
UCLA School of Medicine
Interventional Cardiology Fellowship, Columbia Presbyterian Medical Center
Memberships
Society of Cardiovascular Angiography and Intervention (SCAI)
American College of Cardiology (ACC)