A soft robotic heart that is designed to replace the need for a heart transplant is one of four research projects that have made the shortlist for the Big Beat Challenge initiative—organised by the British Heart Foundation—that awards £30m to a project that seeks to identify a real-world challenge, a significant unmet need or opportunities for innovation in the field of cardiovascular disease. Jolanda Kluin (Translational Cardiothoracic Surgery, University of Amsterdam, Amsterdam, The Netherlands), lead researcher of the project, talks to Cardiovascular News about why a soft robotic heart could address the need for replacement heart in patients with end-stage heart failure.
What are the current challenges of managing patients with end-stage heart failure?
At present, patients have three possibilities—medication, heart transplantation or ventricular assist devices. The medication has to be delivered intravenously, which requires a stay in hospital and the dosage has keep to being increased because it stops having an effect; there is a huge shortage of donor hearts and I do not foresee that current initiatives—such as using hearts of people who have died outside of hospital—leading to a significant increase in the donor pool; and ventricular assist devices are associated with major complications (e.g. device-related thrombus or bleeding because of anticoagulation medication) and poor quality of life.
What is the concept of the soft robotic heart?
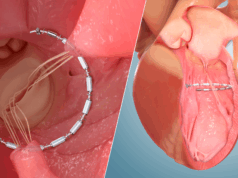
From a surgical point of view, it is similar to heart transplantation because the native heart is removed. We aim to have a soft robotic shell that forms the soft artificial muscles and sensors to enable natural motion, and a tissue-engineered lining to make sure all the surfaces in contact with blood are essentially the patient’s own cells. This means that unlike with ventricular assist devices, a patient will not need to take anticoagulation or least not to the same extent. Furthermore, the energy transfer will be wireless.
What work have you done so far on the project?
Two years ago, we applied and received a €3 million future and emerging technologies grant (part of the Horizon 2020 project) from the European Union. This grant will last five years and with it, we hope to make three prototypes. The ultimate goal is reach the stage at which we are able to do the first implantation in a large animal.
If you win the Big Beat Challenge, what do you hope to do with the money?
We have to conduct a substantial number of experiments to ensure that the soft robotic heart is safe and, at present, we do not have enough researchers to do that. Therefore, the Big Beat Challenge money will fund the project for a further seven years and allow us to do a lot of in vitro work in Mockloop circulations. We will also develop various prototypes—looking at how it beats, how it contracts, and how it works in large animals. At the end of the seven years, we hope to be at the stage at which we can do the first-in-human implantation.
However, £30m will probably not be enough to achieve everything that we want to achieve. Therefore, during the next few years, we hope to be able to encourage companies to invest in the project so that we can continue our work.
Assuming your project is successful and you are able to develop the soft robotic heart for use in clinical practice, which patients do you think will benefit the most?
The greatest need for such a device are infants because very few donor hearts are available for this patient group. There are also young patients with congenital heart disease who cannot undergo heart transplantation. For example, those with pulmonary hypertension. Pulmonary hypertension requires the right ventricle to be strong but the right ventricle of transplanted hearts is not used to beat against high pressures. So at present, their only option is a heart and lung transplant.
The group that is the largest in numbers are adult patient with end-stage heart failure. This can have several causes: e.g. an ischaemic cause or cardiomyopathy. We plan to power the heart transcutaneously (wireless) with no drive line, which may be challenging in a baby (because of their small anatomy). Therefore, we may start in an adult population who are 50 or 60 years of age who have had a big myocardial infarction.