This advertorial is sponsored by Shockwave Medical.
The latest data from the Disrupt CAD clinical study programme, assessing the use of Shockwave intravascular lithotripsy (IVL) in the coronary arteries, provide compelling evidence that the technology is capable of modifying coronary calcium regardless of morphology—including eccentric and nodular calcium—prior to stent implantation. This is according to Javier Escaned (Hospital Universitario Clínico San Carlos, Madrid, Spain) and James Spratt (St George’s University Hospital NHS Trust, London, UK), who tell Cardiovascular News about the challenges of treating both eccentric and nodular calcium and discuss how new findings offer a reassuring picture of the use of IVL in these cases.
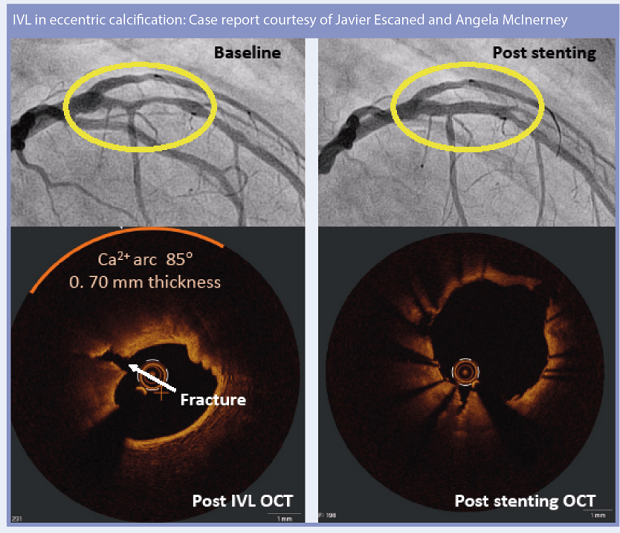
The treatment of eccentric and nodular calcium is seen as being particularly challenging in coronary vessels. The presence of eccentric calcium, whereby plaque volume is more concentrated on one side of the vessel, may cause uneven or incomplete stent expansion, ultimately increasing the likelihood of stent failure. This is particularly evident in the case of calcific nodules, blocks of calcified plaque that typically protrude into the lumen, which in addition to causing suboptimal stent expansion may cause gross malapposition of stent struts against the vessel wall.
Current treatment approaches include balloon-based techniques, rotational atherectomy or orbital atherectomy, while IVL is an emerging treatment technique which uses sonic pressure energy, known as shockwaves, that pass through soft arterial tissue and preferentially disrupt calcified plaque by creating a series of microfractures. “IVL selectively targets calcium, with shockwaves that target the interface between calcium and non-calcific tissues,” says Spratt.
Though IVL’s functionality in concentric lesions is well recognised, new data shed light on its use in treating both eccentric and nodular calcification. “We know that calcification has different patterns in the coronary arteries, and previous studies have shown that the degree of calcification plays a very important role in stent expansion, which at the end of the day, is one of the ways that calcification impacts on suboptimal stenting,” comments Escaned. “There was concern that perhaps the mechanical effect of IVL relied a lot on delivering energy inside a tubular calcific segment, and in an eccentric calcification, the elastic, calcific-free part of the vessel will in a way buffer the effect of the soundburst, of the energy delivered to the calcific components of the stenosis.”
OCT analysis
Two studies presented at the Transcatheter Cardiovascular Therapeutics annual meeting (TCT 2021, 4–6 November, Orlando USA and virtual) are among those to offer the clearest picture yet of the effectiveness of Shockwave IVL in both eccentric and nodular calcium. For the first analysis, researchers used optical coherence tomography (OCT) to analyse pooled data from 262 patients treated as part of the DISRUPT CAD I, II, III and IV studies with either eccentric or concentric calcium. Vessels were grouped depending on the arc of calcium seen.
 “The first thing to say is that it provides you with a level of detail that you do not get from an angiogram,” says Spratt, commenting on the use of OCT in the study, which represents the largest analysis of acute OCT outcomes of any calcium modification treatment. This provides a huge level of detail, he says. Turning to the data, he says that the findings should offer reassurance, due to the high number of patients included. “There are 262 cases, which is a lot of OCT studies, and that gives you more confidence in the finding,” Spratt adds.
“The first thing to say is that it provides you with a level of detail that you do not get from an angiogram,” says Spratt, commenting on the use of OCT in the study, which represents the largest analysis of acute OCT outcomes of any calcium modification treatment. This provides a huge level of detail, he says. Turning to the data, he says that the findings should offer reassurance, due to the high number of patients included. “There are 262 cases, which is a lot of OCT studies, and that gives you more confidence in the finding,” Spratt adds.
The analysis confirmed that coronary IVL achieved an excellent minimum stent area (MSA) and stent expansion (SE) consistently in lesions with both eccentric and concentric calcium. MSA and SE at the maximum site of calcification were similar across the four calcium arc quartiles analysed: ≤180 degrees (6.1mm2 and 104%), 181‒270 degrees (6mm2 and 101%), 271‒359 degrees (6.1mm2 and 98%) and 360 degrees (6.2mm2 and 105%), respectively.
Among the key aspects of the study is the relationship between the number of fractures seen in the calcium, relative to the type of calcium present, and the impact this may have on MSA and SE. Both Escaned and Spratt note that a greater number of fractures were seen in lesions with a greater degree of calcification.
“Of course, you have a much wider region to find cracks, if you have 360 degrees than if you have 90 degrees, for example,” comments Escaned.
In other words, according to Spratt, “the more calcium, the more fractures”. However, interestingly, Spratt notes that there did not seem to be a relationship between the number of fractures and stent expansion. “When you did not see the fracture, it did not seem to affect how well the stent expanded, which was a little bit of a surprise,” he comments.
This is a point echoed by Escaned, who adds: “What is important is that if you divided into those that you see fractures and those that you do not see fractures, with all these different groups of calcification, there were no differences between groups and no differences between the presence or absence of fractures in terms of MSA, or in terms of SE.”
Important lessons
Another learning point from the study, highlighted both by Escaned and Spratt is the mismatch between the location of the vessel with the most calcium and the narrowest point of the vessel.
 “What was found within the study was that the area that was narrowest was not the area with the highest calcium,” says Spratt. “That shows you a behavioural effect that where we see severe narrowing we often concentrate all of our treatment at these severe narrowings and ignore bystander areas,” he adds.
“What was found within the study was that the area that was narrowest was not the area with the highest calcium,” says Spratt. “That shows you a behavioural effect that where we see severe narrowing we often concentrate all of our treatment at these severe narrowings and ignore bystander areas,” he adds.
Escaned suggests this is a finding that bodes well for IVL as a treatment modality. “The good thing about this technique is because it is delivering energy to a wider segment than the tightest point of the stenosis, you are already preparing the lesion to perform the proper stent implantation, that is the message here,” he says.
In terms of the robustness of the data, the fact that there were no major differences in the procedural aspects across the subgroups of lesions should provide reassurance, according to Escaned. “It is a very solid dataset, because it was obtained in the context of prospective trials so that means that it is rigorous patient selection, acquisition and follow-up,” he comments. “When you looked at procedural time, contrast volume, predilation, the number of pulses that were delivered, there were no differences.”
An important aspect to consider, according to Escaned, is stent expansion in the four different groups depicting different degrees of eccentricity or concentricity of calcium after IVL. “In these four studies, there were no significant differences in minimal stent area, which suggests that for one reason or the other, from a practical perspective IVL was equally effective in all of these subgroups of lesions”, he comments.
Summing up the totality of the data, Escaned adds: “This is the study that provides, for the first time, evidence suggesting that IVL is, from a practical perspective, equally effective in eccentric and concentric plaque.”
Calcific nodules
In a separate analysis of calcific nodules, coronary IVL was found to have a notable acute effect on calcific nodules, which were identified in 22% of cases, either by flattening or fracturing the nodule, resulting in consistent MSA (6.3mm2 vs. 6mm2) and SE (101% vs. 103%) in lesions with calcified nodules (n=54) or those without (n=194), respectively. The analysis also found that calcific nodules were more commonly associated with concentric calcium and greater overall calcium burden.
“The main feedback in terms of the data was that with eccentric and nodular calcium you can still get good stent results,” says Spratt. “Lithotripsy, prior to the recent data from TCT, was really an unknown. It was really unclear whether it would work, and the initial data are encouraging in that they show that it seems to treat nodular calcium pretty well.”
Escaned describes nodular calcification as “the most extreme” subgroup of eccentric lesions. “Interestingly, the same thing was observed,” he says. “There was a very good result in this group of patients.”
Reflecting on the overall message from each of the studies, Escaned and Spratt say that the new data add positively to the overall understanding of the outcomes of IVL in a range of morphologies.
“I think that the overall message is that for the first time we have objective evidence based on imaging and a solid dataset, that IVL is effective irrespective of the degree of calcification, in terms of the distribution of calcium that we see in the vessels,” says Escaned.
For Spratt, the simplicity and safety of IVL are further benefits. “IVL is a very easy technology to learn,” he comments. “There is no learning curve to it, [and] it is very safe. There is no signal for harm—acute or long-term harm. Those are two great foundational pieces to build an evidence base on and that means that you can try IVL therapy where you are not sure if it will work or not work. That will lead to its expansion into areas where we have been more concerned about a morbidity price to pay.”











