A network meta-analysis, published in JACC: Cardiovascular Interventions, indicates that three contemporary drug-eluting stents—Xience (a cobalt-chromium everolimus-eluting stent; Abbott Vascular), Promus (a platinum-chromium everolimus-eluting stent, Boston Scientific) and Orsiro (a hybrid sirolimus-eluting stent, Biotronik)—all have a significantly lower risk of device thrombosis compared with Absorb (a bioresorbable vascular scaffold, Abbott Vascular).
Writing in JACC: Cardiovascular Interventions, Si-Hyuck Kang (College of Medicine, Seoul National University and Cardiovascular Centre, Seoul National University Bundang Hospital, Seongnam-si, South Korea) and others report that recent studies have shown that Absorb is efficacious as Xience in terms of repeat revascularisation “but safety concerns have been raised as well”. They add that the aim of their study was to further explore the safety of the bioresorbable scaffold by assessing the rate of device thrombosis of various contemporary drug-eluting stents—including the scaffold. “Due to the low incidence rates of stent thrombosis, a very large sample size was required to detect differences in a single trial setting. A network meta-analysis has the advantage of providing comprehensive information by combining data from a complex network of multiple trials. For this purpose, we performed a systematic literature review of randomised controlled trials and updated a multiple-treatment network meta-analysis using a Bayesian framework,” Kang et al comment.
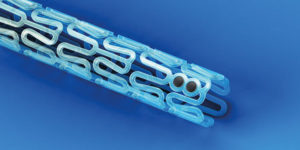
In the network meta-analysis, the authors reviewed 147 trials (including 126,526 patients overall) that assessed different drug-eluting stents. The devices evaluated included bare metal stents, first-generation drug-eluting stents (such as the paclitaxel-eluting stent; Taxus, Boston Scientific), next-generation stents with a permanent polymer (such as Xience and Promus), next-generation stents without a permanent polymer (such as Orsiro), and Absorb. The principal endpoint was the one-year rate of definite or probable stent thrombosis.
According to Kang et al, all of the drug-eluting stents—apart from Absorb and Taxus—were superior to bare metal stents in terms of the primary endpoint. The authors also report that the risk of stent thrombosis was significantly lower with Xience, Orsiro, and Promus compared with Absorb and a (now discontinued) zotarolimus-eluting stent (Endeavor, Medtronic). However, they note their findings should be interpreted with caution because comparison data for some of the devices evaluated in the network meta-analysis, including Orsiro and Absorb, were limited and “some of the studies had a potential risk of bias”. Furthermore, they report that the inferiority of the scaffold (in terms of device thrombosis) “was lost after exclusion of studies with potential risk of bias”.
Reviewing other safety and efficacy endpoints, Kang et al did not observe any statistical differences in the rate of all-cause death or cardiac death between the devices evaluated. “All contemporary drug-eluting stents and the bioresorbable vascular scaffold showed low risks of target vessel revascularisation and target lesion revascularisation. All drug-eluting stents were associated with reduced risks of repeat revascularisation compared with bare metal stents,” the authors state. They add that “in particular” the scaffold had a similar risk for repeat revascularisation as other drug-eluting stents, including Xience, Promus, and Orsiro.
Noting that the complete degradation of the current-generation bioresorbable scaffold is achieved within one to four years, Kang et al comment that the benefit of the device “may emerge after one year post implantation”. They add: “Considering that stent thrombosis occurs in 1% of patients during the first year and then in 0.5% per year thereafter, the benefit, if present, would be paramount.” Therefore, the authors report, extended follow-up of ongoing clinical trials of the scaffold “would provide more insight on this device”. “Results from studies with extended follow-up are anticipated to fully appreciate the long-term safety of contemporary coronary devices,” Kang et al conclude.
In an accompanying editorial, Davide Capodanno (Cardio-Thoracic-Vascular Department, Ferrarotto Hospital, University of Catania, Catania, Italy) comments that Absorb “holds a number of promises but promises are not enough when comparisons versus metallic drug-eluting stents initiate.” He adds that in Kang et al’s study, the device “lost three comparisons (vs. Xience, Orsiro, and Promus) and it “was not proven superior to even bare metal stents and Taxus” (in terms of definite/probable stent thrombosis). However, he adds: “While these results may sound disappointing, more randomised controlled trials with meaningful control arms [he observes that only the comparison with Xience was based on direct evidence] are clearly needed to increase the information size of the Absorb device for the purpose of cross comparisons in future network meta-analyses.”
Capodanno concludes that, given the documented safety and efficacy of contemporary devices at one year, “it is becoming increasingly evident that the real competition—in a landscape of similarly effective devices—will be played on the background of patient safety between one year and the long run.”













