Assessing myocardial viability does not aid the selection of patients who will benefit—or not—from percutaneous coronary intervention (PCI) for the treatment of severe ischaemic cardiomyopathy. This is according to the findings of an analysis of the REVIVED-BCIS-2 trial, in which investigators assessed the effect of myocardial viability, functional recovery and PCI on clinical outcomes in the trial.
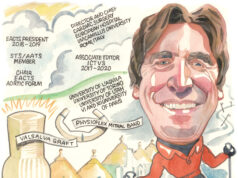
Divaka Perera (King’s College London, London, UK) delivered the findings at the American College of Cardiology (ACC) 2023 Scientific Session (4–6 March, New Orleans, USA), where he commented that the results suggest there is not a “Goldilocks zone” to identify patients suitable for PCI based upon their myocardial viability characteristics.
Perera had previously presented the primary results of REVIVED-BCIS-2 at the annual congress of the European Society of Cardiology (ESC) in 2022 (26–29 August, Barcelona, Spain), where he revealed that there was no reduction in all-cause mortality or heart failure hospitalisation gained through PCI compared to medical therapy among 700 patients with severe left ventricular (LV) dysfunction and extensive coronary artery disease randomised to either approach.
Through their latest analysis, the REVIVED investigators sought to determine the extent to which viability on cardiac magnetic resonance (CMR) imaging or Dobutamine Stress echocardiography (DSE) determines the impact of PCI on clinical outcomes and whether reverse LV remodelling affects clinical outcomes.
Observational data from the latter half of the 20th century have led to the view that viability assessment is a useful tool for picking patients that would benefit from revascularisation, Perera told attendees of ACC 2023, adding that this pointed to the idea that, “if you had viable myocardium classified in a binary way, you do much better with revascularisation than with medical therapy alone”.
Data from the STICH trial, which compared coronary artery bypass graft (CABG) surgery and medical therapy in which around half of patients had discretionary viability testing, appeared to challenge this notion, Perera added. “When those patients were classified once again in a binary way as having sufficient or insufficient viability, those investigators found that it did not seem to predict the benefit of coronary artery bypass surgery, which challenged the prior data,” he said, adding that the STICH investigators also found in a smaller subgroup of that study that those patients that had improvement in LV function did just as well or badly, as those who did not.
This led the REVIVED investigators to test four hypotheses, namely that viability characterisation predicts event-free survival among these patients, that it predicts LV recovery, response to PCI or medical therapy, or that LV recovery predicts event-free survival.
Viability characterisation was assessed in two ways, Perera said, the first based on the potential for recovery—looking at dysfunctional segments—as well as the amount of scar in the heart. All analyses accounted for potential confounders, such as the modality of viability testing and baseline LV function.
Detailing the results, Perera said there was a lack of relationship between dysfunctional but viable myocardium or hibernating myocardium and clinical outcomes. Contrastingly, he said, looking at all viable myocardium, including all the normal segments, there was an interaction, with a hazard ratio of 0.93, with a 7% reduction for every 10% increase in viable myocardium.
Looking at the relationship between scar burden and clinical outcome, Perera said that for every 10% increase in scar volume, there was an 18% increase in the risk of meeting the primary clinical outcome, which he described as a highly significant result.
Dissecting the data by treatment assignment, Perera said that there was no impact of viability assessment in terms of hibernating myocardium or scar burden on the effect of PCI versus medical therapy versus alone.
On ventricular recovery, Perera said that there was a median change of 4.7%. “What we see is that if you look at all viable myocardium, it does predict recovery of LV function, and if you look at scar burden it does the reverse: the more scar you have the less likely you are to recover,” he commented. Hibernating myocardium does not predict LV recovery, he added, describing this as an interesting result.
“We have shown that characterisation by viability assessment does not allow us to select a group of patients who benefit from PCI over medical therapy,” Perera remarked during the concluding comments of his presentation.
“We have also found—and this is perhaps surprising as it challenges the whole theory of hibernation—that the abundance of dysfunctional yet viable segments is not yet associated with prognosis or even with LV recovery,” he said.
Characterising myocardium in terms of scar or the extent of non-viable myocardium, is highly predictive of prognosis and the likelihood of LV recovery, Perera added, noting that this is independent of LV ejection fraction. “In fact, if you were to correct LV ejection fraction for scar it is no longer associated with outcome or LV recovery,” he noted.
“Similar to the initial REVIVED Trial [this] challenges many long-held beliefs in our profession,” Sunil Rao (NYU Langone Health, New York, USA) said in discussion that followed the presentation at ACC. Rao asked Perera to expand on how the data inform understanding definition of hibernating myocardium.
“I think it challenges it,” Perera said in response to this question. “We had come to use viability tests as a prospective marker of hibernation and that is predicated on an assumption that we can pick the parts of the ventricle that recover, or on a whole patient level, the patients that are going to have LV recovery. Using those very metrics that are currently used, we have shown that that does not predict LV recovery. I think we need to challenge the paradigm, and hibernation as we have known and used it does not seem to be valuable in clinical practice anymore.”
Rao also asked whether, in patients with LV dysfunction who have concomitant coronary artery disease, the decision to revascularise should viability testing continue, and if not how should the data should inform decision-making as to who should get revascularisation?
“Unequivocally, no,” was Perera’s response to the question of continuing viability testing to guide patient selection for revascularisation. “There is absolutely no evidence from this or from the STICH viability data that viability testing predicts a group of patients who benefit, and that challenges what we would do in our multidisciplinary team meetings week on week.”
But, Perera said he did not see this as justification to “throw out” viability testing altogether. “We need to change the way in which we use the viability tests, it should not be focused on dysfunctional segments with the prospect of recovery, and we should not link recovery as the only mechanism of benefit, but instead in those very viability tests that we do is embedded really useful information—scar and non-viable myocardium.” Whether this can be used to stratify patients better will need to be tested in future trials, he said.