Robert Wood Johnson University Hospital (RWJUH) and Rutgers Robert Wood Johnson Medical School (RWJMS, both New Brunswick, USA) have been awarded a US$2.4 million grant from the National Heart, Lung and Blood Institute (NHLBI) to develop new technology to better manage patients presenting with heart attacks.
According to Partho Sengupta, Henry Rutgers professor and the chief of cardiology at RWJMS and RWJUH and principal investigator for the four-year study, scores that can predict the risk of a future cardiac event in patients presenting with heart attack were developed nearly two decades ago and do not include current imaging technology in their calculations.
Sengupta and his team believe that data gathered from this study will help clinicians and hospitals develop high-precision decision support tools for early identification and referral of high-risk patients with heart disease for individualised care at centres of excellence in heart and vascular care.
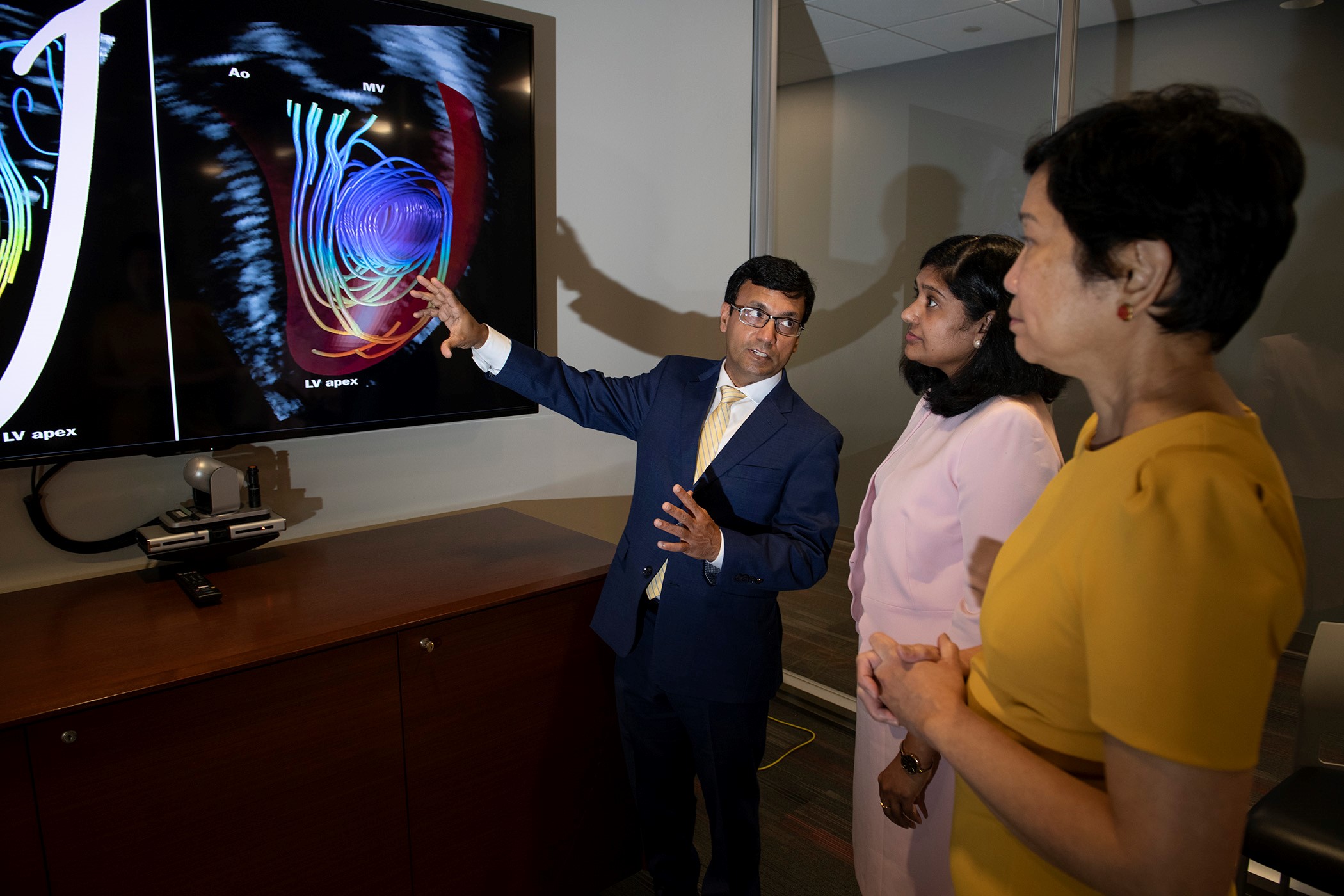
“The current risk calculations were developed prior to the modern therapies we have today,” Sengupta explains. “By conducting this study, we will use artificial intelligence techniques to develop software that can automatically extract quantitative imaging features from the ultrasound images of the heart to identify patients with a heart attack who are at high-risk of death or developing complications.”
There are three primary goals of the study. First is to develop a more accurate risk calculation tool using AI-based imaging features that predict complications from a heart attack or risk of death.
Second, is to use this technology to identify non-ST elevation myocardial infarction (NSTEMI) patients who aren’t transferred initially to a cardiac cath lab because there is no significant irregularity or elevation of their ST reading on an electrocardiogram. NSTEMI has been considered a less serious form of heart attack where there may be partial blockage of a coronary artery, leading to reduced blood flow to the heart muscle.
“However, modern data states that an estimated 30-40% of NSTEMI patients have more seriously occluded (blocked) arteries that are missed by the ECG,” Sengupta notes. “The goal is to get these patients to the cath lab earlier to open their arteries and avoid more damage to the heart muscle.”
Finally, Sengupta believes the ultrasound-based information at the bed side that researchers gather will provide information similar to what is currently produced by magnetic resonance imaging (MRI). The investigators have been recently granted a patent on this technology.
“MRI is not accessible to patients everywhere,” Sengupta says. “Ultrasound is more widely available. Our preliminary clinical data support that cardiac ultrasound radiomics—a mathematical framework that converts standard of care cardiac ultrasound images into minable high-dimensional data—can identify patients at high risk for hospitalisation for serious cardiac events.”
Sengupta notes that this study will involve collaboration and sharing of data among several RWJBarnabas Health Heart & Vascular programs, including Esad Vucic, an imaging specialist in the field of echocardiography and advanced cardiovascular imaging at Newark Beth Israel Medical Center. Vucic will serve as consultant and provide research training for residents and fellows across multiple hospitals.
Sabahat Bokhari, professor of medicine, director, advanced cardiac imaging at RWJMS and director, The Cardiac Amyloidosis and Cardiomyopathy Center at RWJUH; and Naveena Yanamala, associate professor of medicine and section chief and director of research and innovation at RWJMS; are co-investigators for the study.













