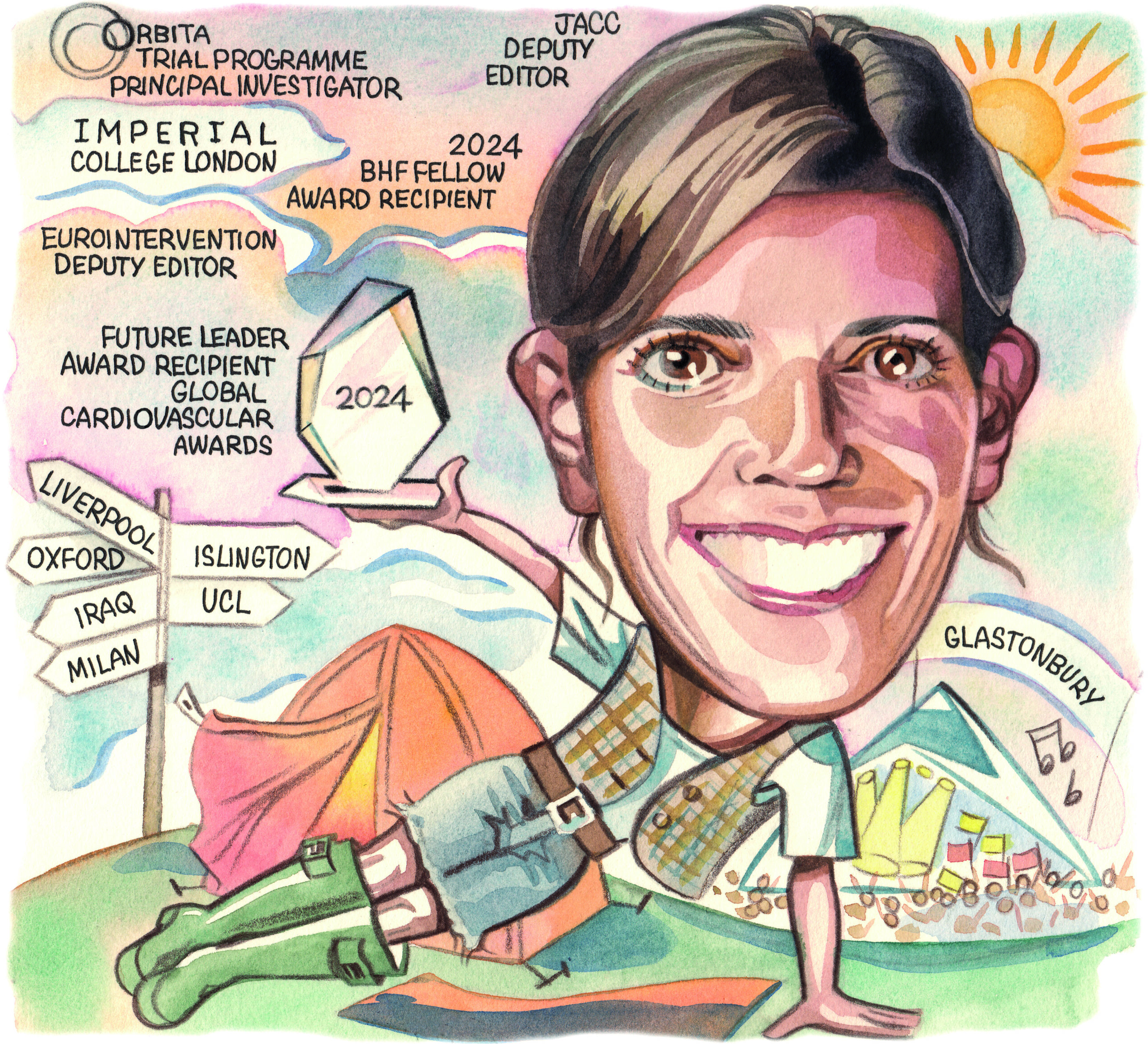
Best known for her work as the principal investigator in the ORBITA trial—a placebo-controlled trial showing that stenting did not improve exercise tolerance or chest pain any more than a sham procedure—Rasha Al-Lamee (Imperial College London, London, UK) talks to Cardiovascular News about the history of the trial and how it has influenced a series of subsequent studies in the treatment of stable coronary artery disease.
Why did you start a career in medicine and what drew you to interventional cardiology?
I come from an Arabic family where your main options are medicine or engineering! I was encouraged to think about medicine as I was good at science, but I was actually quite reluctant to jump into it at first. At school I did basic work experience in multiple things that were not medically oriented, until I finally went and did some shadowing in a hospital and, in that moment, I realised that this was the career I wanted, despite having tried desperately hard to avoid it.
I like talking to people and I am very comfortable with organised chaos. There are so many different opportunities in medicine and every day looks different. You can’t predict how a day will end and that is why I still enjoy it.
Cardiology was the first placement I did as a clinical student in my fourth year at medical school, and I immediately saw that this specialty offers the opportunity to fix people. I toyed with various interventional specialities, but I knew that I wanted to do something very acute so interventional cardiology was the best fit for me.
Who have been the biggest influences on your career?
I have been really lucky to have lots of different mentors at different times. I did a fellowship in Milan with Antonio Colombo and learned a lot about complex angioplasty. My PhD supervisors were Justin Davies and Darrel Francis who taught me a lot about clinical trials and academia. There are a lot of people I rely on for mentorship; Nick Curzen, David Newby, Roxana Mehran and Manesh Patel are just some of the clinical trialists and academics I have to thank for wise words and advice over the years.
What has been the biggest change to the field of interventional cardiology in the time that you have been practising?
When I first started, the only way you could learn about a clinical trial was to be interested and engaged in finding a publication or reading the entire contents of journals like the New England Journal of Medicine or The Lancet. Now the output of research is delivered all day long in bite-sized pieces.
Interventional cardiology has always been a very evidence-based specialty and that has always been a key part of what has driven me to it. Now we are probably one of the leading medical specialties in the application of research, using it to guide our practice and in being quick to adopt or abandon technologies based on the evidence. In my mind, we talk about research in our daily practice far more than many other medical specialties. We have quite a deeply ingrained partnership with industry, that helps to make our specialty faster moving due to more financial investment.
What I am most excited about is that teams that weren’t traditionally academic are now engaging in research. The application of evidence and use of new information has become much more inclusive and it is easy for everyone to have knowledge of what is new and how it might change our practice.
What is the background of the ORBITA trial?
Towards the end of my training as a fellow in cardiology I started thinking about doing a PhD and what the question could be. One day I was in the cath lab having just done an angioplasty for a patient with stable angina, with Darrel Francis supervising the case. I felt that we had achieved a nice result, but Darrel asked, “How do you know it is going to make them feel better?”. That started us thinking about how we answer the question and led to the design of ORBITA.
The main challenge was to get any form of funding. Grant funders and industry thought it was either not an important question, something that was impossible to do, or perhaps they didn’t have personal interest in funding it. We managed to get internal funding from the Imperial Biomedical Research Centre to fund ORBITA.
Then it was about trying to get sites who were up for recruiting into the trial. From the five original sites, all of the principal investigators were people I had trained with or somehow knew and they were all up for doing something really innovative.
The next challenge was to get an ethics committee to agree to a placebo-controlled trial, and they were brave and prepared for the challenge, because they thought, “Why has this not been done before?”. They helped in shaping the patient information literature and the GP literature so that the reasons for taking part and the potential risks were clear.
After that we had to convince patients to be a part of the trial. We recruited almost 60% of the patients we approached, and I was involved in the recruitment of every one. It was a lot of work, and it took four years to do.
The results of ORBITA initially provoked a great deal of controversy and debate—what lessons did you learn from having been at the centre of this?
By nature, I am a person who likes to be liked, and this was the first time I had really been in the limelight. With some of the most eminent people in the field being negative about the result, it was hard to take. There were many points at which I thought I should give up, but the moment I decided not to was in January 2018. We hosted a presentation evening for all the patients enrolled in the trial where I presented the results. During my presentation, one of the patients asked for the microphone, and he shouted out, “Next time you present your results, take us with you!”. That was enough to make me realise that I owed it to the patients to continue to disseminate the results.
One important thing I have learned is that your academic output doesn’t sit in a silo, there can be a real impact of what you do. I am very proud of the impact that ORBITA had and because it delivered a result that was unexpected it has triggered far more research about stable coronary artery disease than it would have done had it delivered the more predicted result.
In that period I think I was very apologetic of ORBITA; now I don’t see any reason to apologise. We learned a lot from ORBITA, and it is the reason we have been able to do more research that tries to answer more questions.
What is coming next from the ORBITA programme?
I think I imagined that ORBITA would be one trial and done. But, in the world of stable coronary artery disease and angina there is a lot to think about, and this is where my group is focused for now. We have learned that angina is complex and its relationship with ischaemia is not as straightforward as we thought. Some of that might explain why, even with good revascularisation, we don’t get the perfect symptom results that we might expect.
 I have built a great team of researchers who I am very proud of. My group are now quite focused on the story around residual angina and most recently we studied the complex population with refractory angina in the ORBITA-COSMIC trial.
I have built a great team of researchers who I am very proud of. My group are now quite focused on the story around residual angina and most recently we studied the complex population with refractory angina in the ORBITA-COSMIC trial.
The next studies you will hear about are ORBITA-FIRE and ORBITA-MOON which are studying the invasive physiological threshold for angina, and if it is possible that different lesions in different vessels contribute to symptoms in different ways. There are also a lot more data coming out from ORBITA-2 and ORBITA-COSMIC, trying to look at the predictors of response in those trials. And of course, we are beginning to plan ORBITA-3 so watch that space.
More broadly I am interested in the application of placebo control in interventional trials, so I am working with lots of groups to think about how we can apply that ORBITA placebo-control methodology and our patient reporting outcomes ORBITA-app, not just to interventional cardiology but to the wider medical world.
Has ORBITA demonstrated the value of placebo-controlled trials in interventional cardiology?
I hope so and I think this is a much more powerful and impactful legacy than the actual trial results. Some of the ORBITA methodology has been used to describe how you ideally apply placebo control within a trial. I really hope that it will be used to demonstrate that, even when we think a therapy works and it has been around for a long time, if you retest it using rigorous scientific methodology you might get a different result. There are so many places where I think we need to think about this and where I believe we are performing procedures without enough evidence.
Importantly, we must be prepared to conduct these trials up front with new technologies whose main aim is the improvement of subjective endpoints such as symptoms or quality of life.
You were recently an author of a paper on the role of intuitiveness in medical decision-making, can you explain
this concept?
Another legacy of ORBITA is how we interpret trial results. Fundamentally, I think we often work backwards from the result. We read the headline and, if it confirms our preconceived belief of how something works, we do not scratch beneath the surface of the abstract. If the result is not one we like, we look much more deeply and search for limitations within the trial, so that we can find an excuse for the unexpected result.
We started to think about why we do that. Sometimes it is just because we have a very dogmatic approach to our understanding of the mechanism of action. If it makes total sense, we are happy to accept less scientific rigour in the data.
Are there any recent trials that have caught your attention?
DanGer Shock really spoke to that story of trying to get to the end of a very difficult trial and the challenges around that process. The investigators are really to be commended for completing the trial and getting the result out there.
I have also been very impressed with how the investigators have been very balanced about how they present their results and consider its potential impact on clinical practice. They have not run away with the results and have tried very hard to discuss which population it might apply to so that we don’t extrapolate the data too far.
What does your life outside of medicine look like?
I’m a proud mum of a 13-year-old who is sports obsessed, so my husband and I spend a lot of time dropping him to various sports practices and matches. One of the things that I have really taken to over the last few years is lots of regular exercise because it is time to myself, and I try to dedicate some time to that every day. Beyond that I have a fantastic family and lots of close friends who are very important to me. I wouldn’t say that I have time for hobbies per se, but I really value the time I get to spend with them.
Every year my husband and I go to Glastonbury. We have been married for 18 years and he is a massive support to me. Once a year we like to go and sit in a field in Somerset and forget about work. For someone like me whose job is really intense, it is about as far away from interventional cardiology as you can get.
Fact file
Current appointments
Cardiology consultant, Imperial College Healthcare NHS Trust
Clinical reader, National Heart and Lung Institute, Imperial College London
Deputy director, Imperial College London School
of Medicine
Co-director of Cardiovascular theme of National Institute for Health and Care Research (NIHR) Imperial Biomedical Research Centre
Cardiovascular speciality lead, NIHR Clinical Research Network (CRN) North West London
British Heart Foundation Intermediate Research Fellow
Deputy editor, EuroIntervention
Deputy editor, Journal of the American College of Cardiology (JACC)
Education and Training
MA (Hons) Physiological Sciences and Preclinical Medicine, St Hugh’s College, Oxford University, Oxford, UK
PhD, Imperial College London, London, UK
MBBS (Lond), Royal Free and University College London Medical School, London, UK
Fellowship training, Hammersmith Hospital, London, UK
San Raffaele Hospital, Milan, Italy













