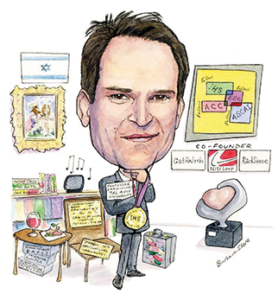
Ran Kornowski (Department of Cardiology, Cardiac Catheterization Laboratories, Rabin Medical Center, Tel Aviv University, Tel Aviv, Israel) talks to Cardiovascular News about his career mentors, his research interests, and his role as president-elect of the Israeli Heart Society. He also talks about his most memorable patient—a man who saved hundreds of Jewish people from the Nazis during the Second World War.
Why did you decide to go into medicine and why, in particular, interventional cardiology?
Medicine has been my desired profession since I was a teenager. I was fascinated by the ability to help people in need and was also very much attracted by the science and innovation involved in medicine. As a medical student, I was stunned by cardiology in general, and by interventional cardiology in particular, after observing a catheterisation procedure for the first time. I interviewed a patient with chest pain during my internal medicine rotation in 1985 and accompanied him to observe his catheterisation procedure. He had tight obstructive left main coronary artery disease and I distinctly remember thinking: “This is it. This is what I want to do!”
The rest of my career has been devoted to achieving my professional goal of being an academic cardiologist and an interventional cardiologist.
Who have been your career mentors and what advice of theirs do you still remember?
I am fortunate enough to have had several outstanding physicians for mentors. Dr Yoram Levo (head of the Internal Medicine Department, Tel Aviv Medical Center, Tel Aviv, Israel) identified my passion for cardiovascular medicine early on and allowed for my foray into research during residency. Dr Gad Keren trained and instructed me at the cardiology department of Tel Aviv Medical Center between 1994 and 1996 and contributed significantly to my clinical and academic career.
It would be remiss of me not to mention Dr Alex Battler, with whom I made my first steps in the basic research laboratory. Later on, he asked me to join the Rabin Medical Center and to become the youngest chief of interventional cardiology in Israel. This opportunity is the reason I left Washington DC with my family in the year 2000. It has also shaped my national and international career during the last 16 years.
There is no doubt that Dr Martin Leon has most profoundly impacted my career. He trained me at the Washington Hospital Center between 1996 and 1998, which was followed by a faculty position as head of experimental revascularisation at the centre between 1998 and 2000. I truly believe I would not be where I am today without his guidance and the opportunities he afforded me. I have learned so much from him and we have maintained a close relationship throughout the years. He is not just a mentor but also a close personal friend.
I also have to mention Stephen Epstein with whom I worked closely in the basic research laboratory. I formed my basic research skills working alongside him. Lastly, over the course of the last decade, I was fortunate to serve as a board member of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) and EuroPCR throughout the directorship of Dr William Wijns. I am constantly inspired by Dr Wijns’ exceptional attitude towards cardiovascular research and education.
During your career, what has been the most important development in interventional cardiology?
In my view, it has been the invention of the catheter-based techniques for cardiac valve implantation. The transcatheter aortic valve implantation (TAVI) revolution is probably the first step, and the entire field is heading towards more research and expansion—we have yet to see the full impact of this revolution.
Aside from that, I have been fortunate to witness and become involved in multiple changes and improvements in interventional cardiology over the last 20 years. Among them have been the introduction of improved stents and drug eluting stents, atherectomy devices, intravascular imaging of coronary lesions and physiology assessment tools. I have also seen intra-procedural and post procedural pharmacotherapies improve. Overall, cardiac patients can now be treated more efficiently and safely compared with the past.
What has been the biggest disappointment? Ie. Something you thought would change practice but did not?
In the late 1990s and through the early 2000s, I conducted with my co-workers a great deal of research in the field of intra-myocardial therapeutics. Specifically, our group pioneered the transcatheter laser direct myocardial revascularisation technique but failed to show any therapeutic benefit in a large blinded randomised trial. Soon thereafter, we worked on the experimental concept of progenitor cell transplantation and gene-based intra-myocardial therapy to promote therapeutic angiogenesis and/or myocardial regeneration among patients with refractory myocardial ischaemic and/or ischaemic cardiomyopathy. I was fascinated by the scientific research and became intimately involved with the translational work needed. My hope was to carry this therapy over from the research lab to the clinical arena for the benefit of cardiac patients. However, after several years of research, the economic crisis of 2007/8 hit and this drained our research budget. I believe this field will revive again as there is still plenty of high-quality research activity. I hope to be part of this renaissance in the near future.
Of the research you have been involved with, what do you think has had the biggest impact on clinical practice?
I have contributed to the field of TAVI by initiating the international valve-in-valve registry that was later branded as the “VIVID registry”. Back in 2009, I performed my first valve-in-valve TAVI procedure at our department and was stunned by the profound and immediate clinical impact of the procedure. At the time, there were no systematic large-scale data about the technique.
Therefore, I initiated a global registry to document and monitor the characteristics and outcome measures of the valve-in-valve procedure. The VIVID registry, currently headed by Danny Dvir (an ex-fellow of mine who now works in Vancouver, Canada), have become an important project and data from the registry has appeared on multiple publications, including JAMA, JACC and Circulation. I am proud to say we incepted this project at Rabin Medical Center before expanding elsewhere.
What are your current research interests?
I am involved in multiple research projects but for brevity’s sake, will focus on two. I am currently exploring a new method that empowers angiograms so we can obtain fractional flow reserve (FFR) data. It is done without a pressure wire and/or infusion of adenosine and was developed at our medical centre as a translational bio-mechanical project. The initial clinical validation was very promising and we launched a start-up company—CathWorks— to further promote this technology. Hopefully, it can become commercially available for everybody soon.
In the basic research laboratory, our team is working on a mice model that allows, by a specific mutation of the αMUPA allele, a spontaneous restriction of the caloric intake causing profound weight reduction and extended animal longevity. We investigated the response of the mutated animals to ischaemic myocardial injury and found the mice to be less susceptible. We also dived into the basic mechanism of cardio-protection in those animals and found it mediated through endogenous leptin pathways. We are very excited about these findings, which may have therapeutic implications.
As well as CathWorks, you have co-founded two other start-up companies. What have been the main benefits and challenges of these experiences?
I have consulted on several start-up companies, as well as capital venture and private equity firms, for many years in Israel and abroad. Eventually, I lost interest in consulting and decided to start my own companies. I teamed up with smart engineers to promote some of my ideas. I co-founded CathWorks, for example, after I recognised a true medical need—eg. angiography-based FFR.
The second start-up company, NitiLoop, has developed a unique catheter-based solution for chronic total occlusion recanalisation and the third, RadSense, focuses on achieving a precise radial artery patent haemostasis following catheterisation. I am also involved with another company dealing with an aesthetic hair-transplant technique.
I find it challenging to convert an idea or even a solid patent into a company. It takes a lot of effort and expertise. It is also heavily dependent on investors and the specific business model. The most gratifying part of the entrepreneurial work is witnessing a theoretical concept becoming a clinical reality, while keeping in mind that the safety of patients always comes first.

You are the president-elect of the Israeli Heart Society. What are your goals for the society?
My first goal is to deliver a message of commitment to the highest quality of care among all members of our society. Second, I intend to maintain—if not strengthen—our international relations with the professional societies and colleges around the wold. The president of the Israel Heart Society is a sort of “foreign minister” for our professional community and I will do my best to represent our society before our international collaborators.
Lastly, I am going to invest in the next generation of cardiologists in Israel, promoting their professional education, expanding their training options and helping to build their careers for the benefit of our patients. I also intend to initiate campaigns to improve the lifestyle of the Israeli population, encouraging people to quit smoking, take up regular exercise, and adopt healthy diet habits.
You have worked in the USA as well as in Israel. Did you see any differences in the way that interventional cardiology was practised?
Most interventional cardiologists in Israel, including myself, were trained in the USA or in Canada. However, many of them are deeply influenced by European practices. The result is a hybridisation of Europe and North America with mutual influences and some important local adaptations and contributions. There are outstanding interventional cardiologists in Israel, using advanced technologies and techniques in most catheterisation laboratories across the country.
We are a population of eight million people with some 30 catheterisation labs across Israel, performing some 48,000 catheterisations a year with a 50% percutaneous coronary intervention (PCI) rate. Israel has an advanced interventional cardiology programme for acute coronary syndrome patients, which has led to intense quality improvement over the last decade with in-hospital mortality figures dropping from 8% to less than 4% among ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI) patients. We have a periodic national survey to monitor and document our acute coronary syndrome results (ie. ACSIS project). We have conducted a multicentre TAVI registry showing excellent results and interesting temporal trends among treated aortic stenosis patients. There are additional outstanding national collaborations in the fields of electrophysiology, chronic heart failure, cardiac imaging and interventional cardiac pharmacotherapy.
What has been your most memorable case and why?
This is a difficult question to answer. There are so many memorable cases that have made a profound impact on me. I have learned from my successes as well as my failures.
However, I will pick one that touched me on a personal level—a 94-year-old male patient who had a successful TAVI procedure indicated for symptomatic aortic stenosis two years ago. During the Second World War, he was the director of a hospital in the Jewish Ghetto of Budapest, Hungary. He was able to save hundreds of Jewish people, children and adults from, deportation to the concentration camps by the Nazis. He told me his amazing personal story during his rehabilitation from the procedure.
A few months later, following his full recovery, his grandson sent me a link to the Yad Vashem website (www.yadvashem.org). Each year, during the official Holocaust Martyrs’ and Heroes’ Remembrance Day ceremony (5 May in 2016) that takes place at Yad Vashem, six torches representing the six million Jews murdered during the War are lit by Holocaust survivors. My patient was one of the six torch lighters due to his valiant rescue efforts.
I am a third generation to the holocaust. My grandfather was deported from Paris during the war and he was burned in Auschwitz. Therefore, I was particularly moved by my patient’s story of survival and courage and was pleased that my treatment revitalised him.
Outside of medicine, what are your hobbies and interests?
I like to travel and do so as much as possible. I enjoy sightseeing, exploring art, consuming good food and even better wine. I like listening to music, especially jazz and classical music and I am fond of reading books and biographies as well as watching movies and plays. I cherish the time I spend with my family and friends.
My main interest outside of medicine is art, both classic and contemporary. I am an ardent patron of art Institutions, museums and galleries around the world. I read a lot about art and various artists, and I find art to be immensely inspiring.
Factfile
Notable appointments and achievements
- Present—full professor of Cardiology, Tel Aviv University, Tel Aviv, Israel
- Present—chairman of the department of Cardiology and Cardiac Catheterization Institute, Rabin Medical Center, Petach-Tikva, Israel
- President-elect—Israeli Heart Society (presidency to start in mid-2017)
- 2014 and 2016—Two healthcare management courses, Harvard Business School, Boston, USA
- Immediate past chairman of the Israeli Working Group on Interventional Cardiology (Israeli Heart Society)
- 2007–2011—head of the Research Authority, Rabin Medical Center, Petach-Tikva, Israel
- 1996–2001—fellowship/faculty position, Washington Hospital Center, Washington DC, USA. While at the centre, headed a unit that was dedicated to developing novel experimental revascularisation and therapeutics
- Published more than 400 peer-reviewed publications
- Co-founded of three start-up companies: CathWorks, NitiLoop, and RadSense
Societies
- Fellow of the Israeli Heart Society
- Fellow of the European Society of Cardiology
- Fellow of the American College of Cardiology
- Scientific community; Transcatheter Cardiovascular Therapeutics
- Scientific community; Cardiovascular Research Technologies
- Founding board member of EAPCI
- Scientific board member and course co-director of EuroPCR
Selected studies (as first or senior author)
- Usefulness of the CHA2DS2-VASC Score to Predict Adverse Outcomes in Patients Having Percutaneous Coronary Intervention. Am J Cardiol 2016
- Urgent Transcatheter Aortic Valve Implantation in Patients With Severe Aortic Stenosis and Acute Heart Failure: Procedural and 30-Day Outcomes. Can J Cardiol 2016
- Long-Lived αMUPA Mice Show Attenuation of Cardiac Aging and Leptin-Dependent Cardioprotection. PLoS One 2015
- Outcomes of Patients at Estimated Low, Intermediate, and High Risk Undergoing Transcatheter Aortic Valve Implantation for Aortic Stenosis. Am J Cardiol 2015
- Transcatheter aortic valve implantation in failed bioprosthetic surgical valves. JAMA 2014








