Should interventionalists prioritise native or saphenous vein graft percutaneous coronary intervention (PCI) when treating coronary disease in patients with previous post-coronary artery bypass graft (CABG) surgery?
This was the question at the heart of the PROTCTOR trial, a multicentre, open-label, randomised trial comparing clinical outcomes between the two strategies in post-CABG patients presenting with saphenous vein graft failure.
Ruben W de Winter (Amsterdam University Medical Centers, Amsterdam, the Netherlands) presented one-year outcomes of the study at the 2025 Transcatheter Cardiovascular Therapeutics (TCT) meeting (25–28 October, San Francisco, USA), where he reported that saphenous vein graft PCI in the high-risk and complex post-CABG patient population led to improved one-year clinical outcomes compared with native vessel PCI. The findings of the trial, which was sponsored by Abbott, were simultaneously published in the Journal of the American College of Cardiology (JACC).
“CABG’s long-term durability is limited by both bypass graft failure and progression of disease in the native coronary arteries. As a result, there’s a substantial number of patients that experience recurrent angina symptoms and ischaemia, affecting up to six out of 10 patients at 15 years after surgery,” said de Winter.
“Many prior CABG patients return to the cath lab for repeat coronary angiography and further revascularisation therapy. In patients with previous CABG who require repeat revascularisation, current guidelines recommend PCI of the native coronary artery over PCI of the diseased bypass graft with a class 2A level of evidence B based entirely on observational data.”
In a bid to answer this question, investigators randomised 220 patients with prior CABG and significant saphenous vein graft stenosis one to one to either a strategy of native vessel PCI (n=108) or saphenous vein graft PCI (n=112) at 14 centres in Europe between January 2019 and December 2023.
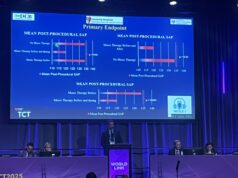
The primary endpoint was one-year major adverse cardiovascular events (MACE), a composite of all-cause mortality, non-fatal target coronary territory myocardial infarction (MI) and clinically driven target coronary territory revascularisation. At one year, MACE occurred in 37 (34.3%) patients in the native vessel PCI group and 21 (18.7%) patients in the saphenous vein graft (SVG) PCI group.
No significant differences in rates of all-cause mortality were observed between the two groups (5.6% native vessel versus 3.6% SVG). However, both non-fatal target coronary territory MI (22.6% native vessel versus 11.7% SVG) and clinically driven target coronary territory revascularisation (18.4% native vessel versus 9.1% SVG) occurred more frequently in patients assigned to native vessel PCI.
De Winter commented that the difference in outcomes between the two approaches had been influenced by fewer PCI-related MIs and clinically-driven target coronary territory revascularisation, adding that the results challenge current guidelines at one-year clinical follow-up. Long-term data will be essential to show if the advantage continues for saphenous vein graft PCI continues over time, he said.
Critiquing the paper in an accompany editorial in JACC, Yousif Ahmad (University of California, San Francisco, San Francisco, USA), Rohin Reddy (Imperial College London, London, UK) and Robert Yeh (Beth Israel Deaconess Medical Center, Boston, USA) point to the relatively complex nature of the lesions in the native vessel PCI group, where 83% comprised chronic total occlusions (CTO) and over half of procedures requiring a retrograde approach.