Supporting the results of previous studies, a new study indicates that percutaneous edge-to-edge repair (MitraClip, Abbott) is a feasible approach for high-risk patients with tricuspid regurgitation. Furthermore, for the first time, this study provides insight into which patients may benefit the most from the procedure—finding that tricuspid regurgitation jet is a successful predictor.
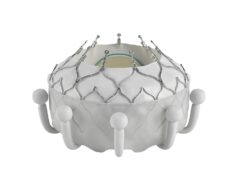
Writing in EuroIntervention, Philipp Lurz (Department of Cardiology, Heart Center Leipzig—University Hospital, Leipzig, Germany) and others report that several transcatheter techniques and devices have been used in patients with tricuspid regurgitation and have been associated with “promising early feasibility results”. They add that of these techniques, edge-to-edge repair technique is the one that has been used most often.
Commenting that a recent study “shed light on patients considered for these interventions”, Lurz et al write: “We here report a single-centre experience of 42 patients undergoing edge-to-edge tricuspid repair treatment with complete clinical and echocardiographic 30-day follow-up and, for the first time, provide predictors for procedural success”.
Of the 42 patients, 31 received a combined tricuspid valve and mitral valve repair procedure; 11 underwent isolated tricuspid repair. The authors report: “Overall procedural success rate—successful clip placement leading to a reduction in tricuspid regurgitation by at least one grade—was 83%. In total, 68 clips were implanted in the tricuspid valve position.”
In both patients who underwent a combined procedure and those who underwent an isolated procedure, significant improvements in New York Heart Association (NYHA) functional class and six-minute walk distance were seen during follow-up (30 days). Of the eight patients (overall) in whom no improvements in NYHA functional class were seen, tricuspid regurgitation remained stable in three patients and changed from “massive” to “severe” in another.
However, according to Lurz et al, no significant change in Minnesota Living with Heart Failure Questionnaire was observed in either patients who underwent the combined the procedure or those who underwent the isolated procedure. Noting that tricuspid regurgitation remained “severe” in 16% of patients in their study, the authors comment that this finding suggests that “there is room for improvement with respect to technical and procedural aspects during tricuspid regurgitation”. “Recent data indicate that after minimally invasive mitral and tricuspid valve surgery, tricuspid regurgitation is reduced to grade 2 or less in more than 95% of cases and, therefore, one should be cautious not to fuel unrealistic expectations when alternative transcatheter options for tricuspid repair are discussed with referring physicians, patients and relatives,” they add.
Additionally, Lurz et al analysed the predictors of success of tricuspid valve edge-to-edge repair—representing the first time that predictors of success of this procedure in this patient cohort has been performed. They found that predominantly non-central tricuspid regurgitation or non-anterospetal tricuspid regurgitation jet appeared as the only significant predictor for procedural failure. The authors comment: “Importantly, in our cohort, clip placement between the anterior and posterior leaflet resulted in unchanged or even increased tricuspid regurgitation in two patients with subsequent clip removal”
Concluding their study, they state that future studies are needed “to address the question of morphological assessment for prediction of procedural success.”
Lurz told Cardiovascular News: “Transcatheter edge-to-edge repair of tricuspid regurgitation is a promising technique but requires refinements of patient selection and procedural techniques.”