Live cases broadcast at interventional cardiology meetings are performed without compromising the safety of patients undergoing the procedures, according to new research presented at the 2024 edition of PCR London Valves (24–26 November, London, UK).
“Live case demonstrations have been a core component of interventional cardiology since the inception of the specialty, and they are a popular feature of pretty much every conference today,” Christopher Allen (Cedars Sinai Medical Center, Los Angeles, USA) told delegates during his presentation on day one of the event.
Whether the educational opportunity that is afforded by a live case justifies any potential safety risk to the patient continues to be a source of debate, Allen said, prompting the analysis looking at procedural safety among 115 live cases. Their researched comprised transcatheter aortic valve implantation (TAVI) and mitral and tricuspid procedures from three high-volume centres over a 14-year period. Researchers compared safety outcomes from the live cases to corresponding clinical trials and real-world daily practice.
“The majority of the cases were TAVI, but there was an increase in the transcatheter mitral and tricuspid interventions over time, as we might expect,” Allen detailed, adding that the cohort were predominantly elderly with comorbidities that reflected a high-risk surgical cohort.
Among the 91 patients who underwent TAVI procedures, the researchers observed a technical success rate of 99%, with a low incidence of vascular injury and major bleeding. Thirty-day mortality stood at 3%, comparable to findings of the PARTNER 2 trial.
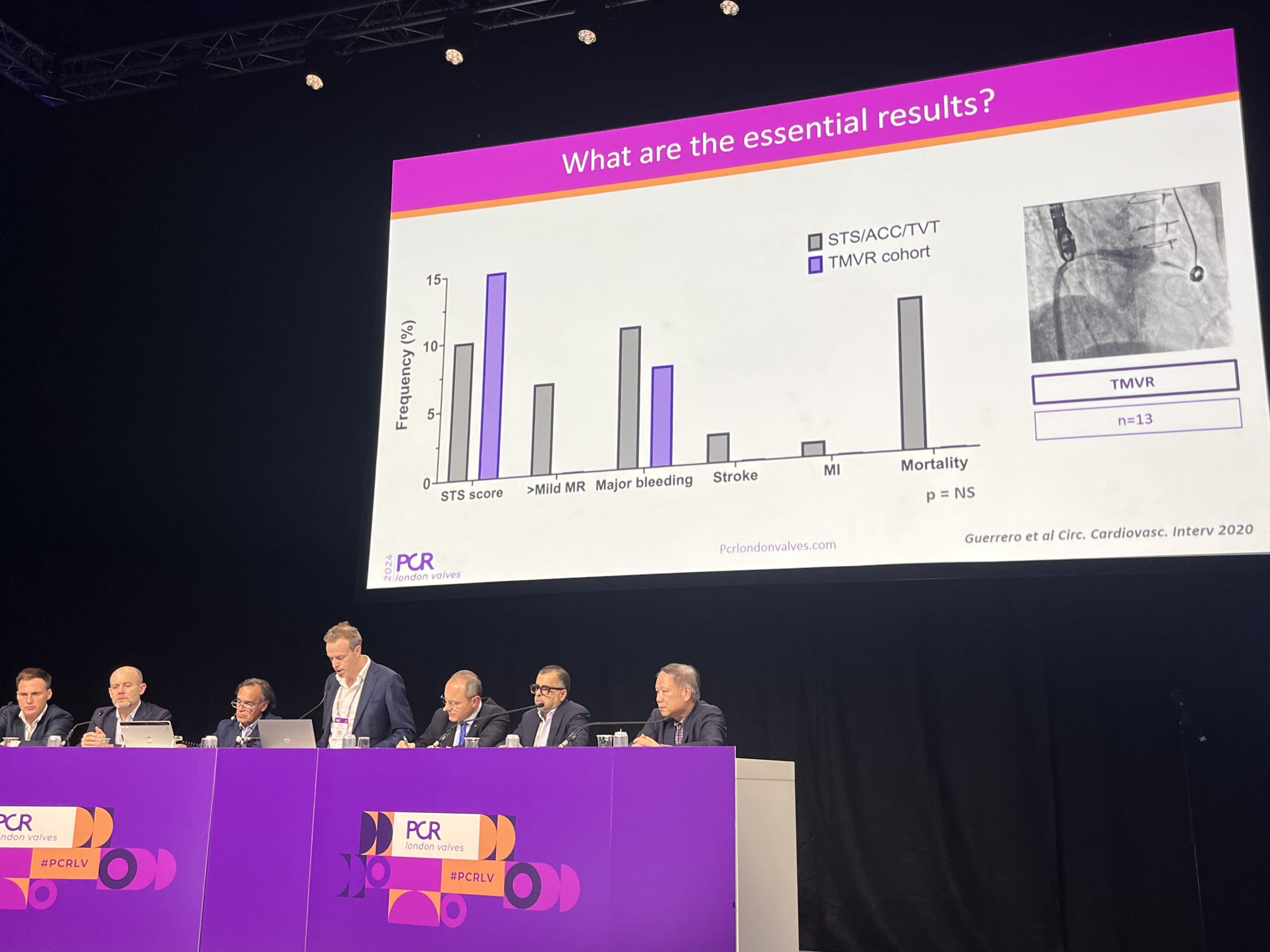
The 13 transcatheter mitral valve replacement (TMVR) procedures comprised a mixture of valve-in-valve, valve-in-ring and valve-in-mitral annular calcification (MAC) cases, with rates of technical success, major complications and mortality at 30 days matching those seen in the Society of Thoracic Surgeons (STS)/American College of Cardiology (ACC). For the six mitral transcatheter-edge-to-edge repair (TEER) cases included in the analysis, technical success matched rates seen in the recent EXPAND G4 registry, Allen detailed.
The daily practice cohort of 346 consecutive patients undergoing TAVI at St Thomas’ Hospital in London over one year were less likely to have undergone cardiac surgery, which together with a decreased frequency of comorbidities meant that they had a lower baseline surgical risk than the live case cohort examined in the study.
“Despite these baseline differences there was no difference in 30-day MACE between the live case and the daily practice cohort,” Allen commented.
“In the present analysis, which is the largest combined experience to date and the first to feature the more recently developed transcatheter interventions, despite a high baseline predictive risk, live cases performed in these experienced centres were associated with excellent outcomes and very low complication rates,” he concluded. “We feel this is important because, in carefully planned cases treated by an experienced team, live broadcast did not compromise patient safety.”










