Given sufficient time, all bioprosthetic valves fail—whether they are surgical or transcatheter devices. The most important predictive factor for bioprosthetic heart valve degeneration is a younger age at implantation. Hence, therapies aimed at delaying the implantation of a bioprosthetic valve are of considerable interest to the field. Darren Mylotte, Antoinette Neylon, and Andreas Baumbach discuss the potential of the novel Leaflex Performer device (Pi-Cardia) to delay, or perhaps negate, the need for bioprosthetic aortic valve implantation.
Transcatheter aortic valve implantation (TAVI) is increasingly being used in lower risk populations—data show that it is at least non-inferior to surgical aortic valve replacement in intermediate-risk patients and studies of TAVI in low-risk patients are ongoing. Therefore, the issue of structural valve failure in TAVI will become increasingly important (given that implantation at younger age is the main risk factor for this event).
A therapy that could delay the need for a bioprosthetic valve—particularly if it could provide a durable reduction in the severity of the aortic stenosis, be performed efficiently via a transfemoral transcatheter route, and provide cost-savings compared to TAVI—would prompt substantial physician interest. Such a therapy could also theoretically be applied to some patients deemed too old or frail for TAVI, replacing balloon valvuloplasty; although valvuloplasty has been proven to be acutely efficient, it is of limited clinical value in the long term.
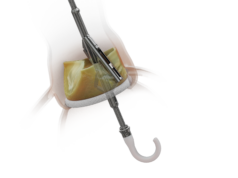
The Leaflex Performer is a transfemoral transcatheter device that uses two unique mechanical structures for scoring aortic valve calcification. The current deflectable transfemoral delivery catheter is inserted via a 16Fr sheath and is delivered and positioned in the aortic root using fluoroscopic guidance. The distal tip of the device features an atraumatic pigtail for safe positioning in the left ventricle and also allows for monitoring of left ventricular pressure. The device itself consists of a proprietary expander placed in the left ventricular outflow tract that lifts the aortic leaflets into contact with three scoring arms positioned in the aortic root. Mechanical expansion of expander yields directed scoring of calcifications within the leaflets, and rotation of the arms allows scoring to be performed at different sections of each aortic valve leaflet.
The design of the Leaflex Performer was based on extensive bench and imaging research on the patterns of calcium distribution in human aortic valves. These analyses revealed two distinct patterns of calcification: bridge and half-bridge. Successful scoring of the calcium has been demonstrated to improve valve area and transvalvular gradients on the bench. The Leaflex technology and mechanism of action is fundamentally different from the traditional balloon aortic valvuloplasty, whereby the annulus and supporting anatomy are simply stretched thus yielding short-term haemodynamic improvement. Indeed, one could also envisage the Leaflex technology being used to prepare heavily calcified or bicuspid valves for optimal implantation of a transcatheter heart valve.
At EuroPCR (22—24 May, Paris, France), Boguslaw Kapelak and Krzysztof Bartus (both Department of Cardiovascular Surgery and Transplantology, Jagiellonian University, John Paul II Hospital, Krakow, Poland) reported safety and efficacy of leaflets scoring during traditional open surgery. The first enrolment in the transfemoral first-in-human study was presented by Darren Mylotte (University Hospital, Galway, Ireland) at PCR Innovators Day (21 May, Paris, France). He reported successful insertion, delivery, functionality, and removal of the device. Moreover, invasive haemodynamic assessment suggested a significant reduction in transvalvular gradient after scoring the calcified aortic valve on four occasions (per protocol). Study enrolment is ongoing in several European centres and further results are eagerly awaited.
In summary, a non-implant based treatment of aortic stenosis is desirable and may have exciting potential once safety and efficacy is demonstrated.
Darren Mylotte and Antoinette Neylon are at University Hospital and National University of Ireland, Galway, Ireland; Andreas Baumbach is at Barts Heart Center, London and Queen Mary University of London, London, UK.