Analysis of data from the Society of Thoracic Surgeons (STS) and American College of Cardiology (ACC) TVT registry, charting early US commercial experience with the Evoque (Edwards Lifesciences) transcatheter tricuspid valve replacement (TTVR) system, has demonstrated favourable short-term safety and effectiveness of the device, according to investigators.
Rahul Sharma (Stanford Unversity, Palo Alto, USA) presented 30-day clinical and quality-of-life data from the first 1,034 patients treated with Evoque in the USA in a late-breaking presentation at the 2025 Transcatheter Cardiovascular Therapeutics (TCT) meeting (25–28 October, San Francisco, USA), describing the findings as “very reassuring”.
Evoque was the first tricuspid valve replacement system to receive US Food and Drug Administration (FDA) approval for the treatment of tricuspid regurgitation (TR), when it was approved in February 2024, indicated for the improvement of health status in patients with symptomatic severe TR despite optimal medical therapy, for whom tricuspid valve replacement is deemed appropriate by a heart team. This came after CE-mark approval in October 2023.
The system is comprised of a nitinol self-expanding frame, intra-annular sealing skirt and tissue leaflets made from bovine pericardial tissue, which is delivered transfemorally. “It’s designed to seal within the native tricuspid annulus using both an intra-annulus sealing skirt and the presence of the frame and interaction with the leaflets,” Sharma said.

Six-month results from the randomised controlled pivotal trial, TRISCEND II, presented at TCT in 2023, reported favourable safety and effectiveness outcomes, demonstrating superiority to optimal medical therapy alone and meeting all primary endpoints. Key findings in the trial included significant reduction or elimination of TR and significant and sustained quality-of-life improvement.
Using data from the TVT registry, Sharma and colleagues sought to categorise the procedural, clinical, echocardiographic, functional and quality-of-life outcomes at 30 days among patients who underwent commercial TTVR with Evoque in the US between February 2024 and March 2025.
Patients had an average age of 77 years, Sharma reported, noting that there was a significant number (69%) females treated. Nearly three quarters were New York Heart Association (NYHA) class III or IV, and nearly half had a heart failure hospitalisation in the preceding year.
Sharma noted that the average procedure time stood at around 103 minutes, similar to what was seen in TRISCEND II, with the device successfully implanted in over 98% of patients. A significant proportion of patients were discharged to home with the average hospital length-of-stay at two days, shorter than what was seen in the randomised trial.
Rates of in-hospital and 30-day all-cause mortality stood at 2.3% and 3.1% respectively. Rates of bleeding, meanwhile, at 6.9% in-hospital and 7.9% at 30 days, were lower than those seen in TRISCEND II, Sharma noted.
A “significant” improvement in TR status was seen at 30 days in both unpaired and paired analysis of the data, with the vast majority of patients having non-trace or mild tricuspid regurgitation at the 30-day timepoint. There was a trend towards improved positive right ventricular (RV) remodelling demonstrated by an improvement in end-diastolic mid-RV diameter and RV systolic pressure, Sharma commented of the echocardiographic parameters, adding that tricuspid valve gradients remained acceptable. Similarly, there was a significant improvement in NYHA functional class and Kansas City Cardiomyopathy Questionnaire (KCCQ) scores in patients paired data between baseline and 30 days.
“There are, of course, limitations with a real-world study,” said Sharma. “The echocardiographic assessments were performed by the sites and site-reported without the presence of core lab adjudication. The events themselves were also site-reported with the absence of a centralised clinical events committee review.”
Nevertheless, he commented that the data demonstrate low mortality and heart failure hospitalisation rates seen with the Evoque device.
“The elimination of TR with more than 97% of patients achieving mild or less residual tricuspid regurgitation, significant improvements in functional capacity and quality of life, and lower pacemaker and lower bleeding rates compared to what we experienced in the randomised trial,” Sharma said. “Almost all patients were discharged home with a median hospital stay of two days.”
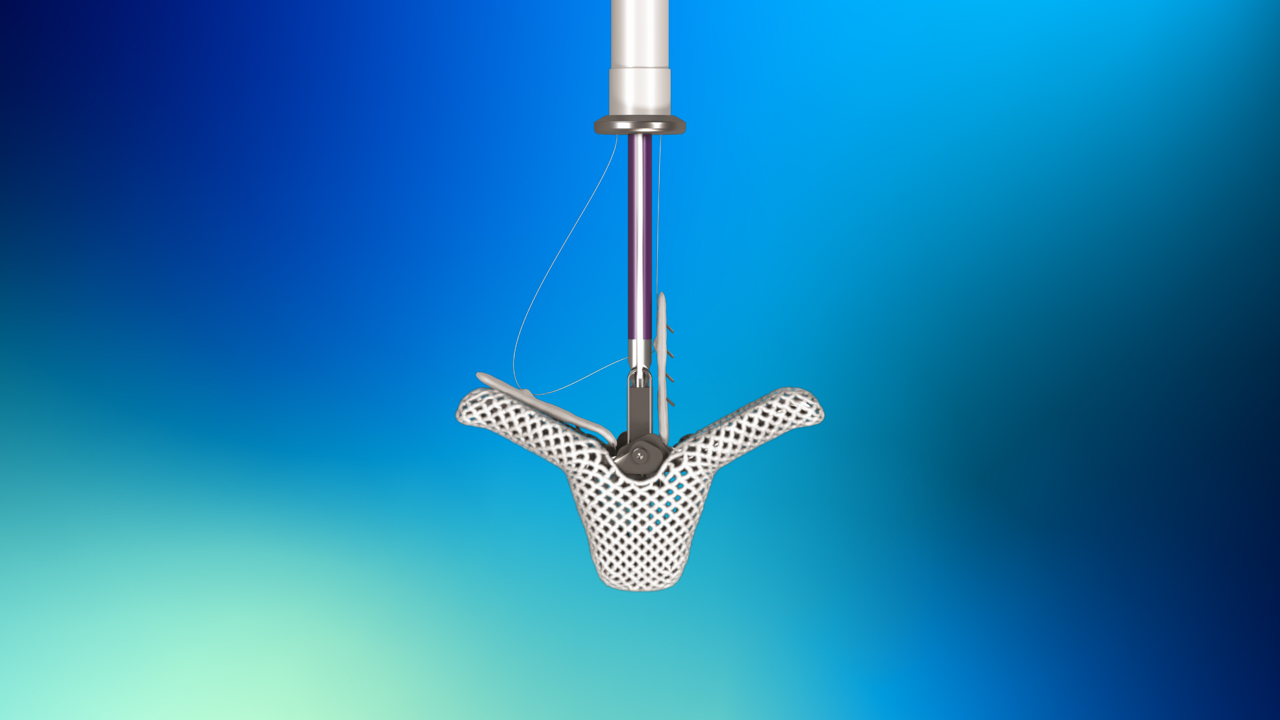
Also at TCT 2025, Jonathan Schwartz (Sanger Heart & Vascular Institute, Charlotte, USA) presented insights from a continued access study of patients who underwent an attempted tricuspid transcatheter edge-to-edge repair (TEER) procedure with the Triclip (Abbott) procedure in the TRILUMINATE pivotal trial. Similar to Abbott’s Mitraclip mitral repair technology, Triclip is a transfemorally delivered system that works by clipping together a portion of the leaflets to repair the tricuspid valve and reduce TR. US Food and Drug Administration (FDA) approval for the system was granted in April 2024, following CE mark in 2020.
The TRILUMINATE pivotal trial, which randomised patients with severe TR either to TEER with Triclip or optimal medical therapy, showed that at two years, patients treated with the device were less likely to be hospitalised for recurrent heart failure than patients, not treated with the device though rates of all-cause mortality in the two arms were similar.
Schwartz presented 30-day follow-up data from patients included in the randomised arm of the pivotal trial, a single-arm trial, and patients enrolled in the continued access study, totalling 847 attempted Triclip procedures.
Detailing the characteristics of the patient cohort, Schwartz reported that patients had an average age of 79 years, 59% were female, 26% had been hospitalised for heart failure within the year prior to their Triclip procedure, and, significantly, 27% had an implantable electronic device.
Implant success was high, with a rate of 98.7%, with patients receiving an average of two devices. Procedure time averaged 146 minutes, with an average of 82 minutes for the device implant. Patients had an average length of hospital stay of one day, with 96.2% discharged to home.
Describing the results as “very reassuring”, Schwartz detailed that around 82% of patients had moderate or less TR at 30-day follow-up, with KCCQ scores improving on average by 17 points from baseline. Adverse event rates were low, with all-cause mortality occurring in 0.5% of cases, major bleeding in 3%, and heart failure hospitalisation in 3%.
“Specifically looking at patients that have electronic devices implanted, this can make the procedure much more complicated, both from an imaging perspective and then navigating around the leads,” Schwartz commented, adding that outcomes among these patients were “very reassuring as well”, with adverse event rates that were broadly in line with patients without implantable devices.
Schwartz also presented analysis stratifying procedural outcomes, adverse events and TR reduction based upon the experience levels of the centres performing the cases, which appeared to show that outcomes improved as the centres gained more proficiency with the procedure.
“As the experience grew, pretty much every category improves,” he commented. “Device times dropped significantly, procedure times down, clip numbers down, intensive care unit [ICU] admissions, adverse event rates, moderate TR or less increased slightly, and TR grade reduction also.”