Economic analysis of the FAME 3 trial, comparing fractional flow reserve (FFR)-guided percutaneous coronary intervention (PCI) to coronary artery bypass graft (CABG) surgery, has shown that CABG incurred higher costs over the five-year lifespan of the trial.
Mark Hlatky (Stanford University School of Medicine, Stanford, USA) presented findings of the analysis at the 2025 Transcatheter Therapeutics (TCT) conference (25–28 October, San Francisco, USA), where he reported that PCI was highly cost-effective compared to CABG, both over five years and in lifetime projections.
The research, also published in the Journal of the American College of Cardiology, shows that patients who underwent PCI returned to work faster than those who underwent CABG, and maintained a higher rate of employment out to five years.
FAME-3 enrolled 1,500 patients in North America, Europe, Asia and Australia, with five-year results, presented at the 2025 American College of Cardiology (ACC) scientific sessions (29–31 March, Chicago, USA) and published in The Lancet having shown no significant difference between the two strategies for a composite outcome of death, stroke or myocardial infarction (MI).
“During the trial we recorded all resource use on electronic forms, including hospitalisations, tests, doctor visits, medications, and we assigned costs to all these resources based on US Medicare price weights,” Hlatky said, outlining the latest analysis at TCT 2025.
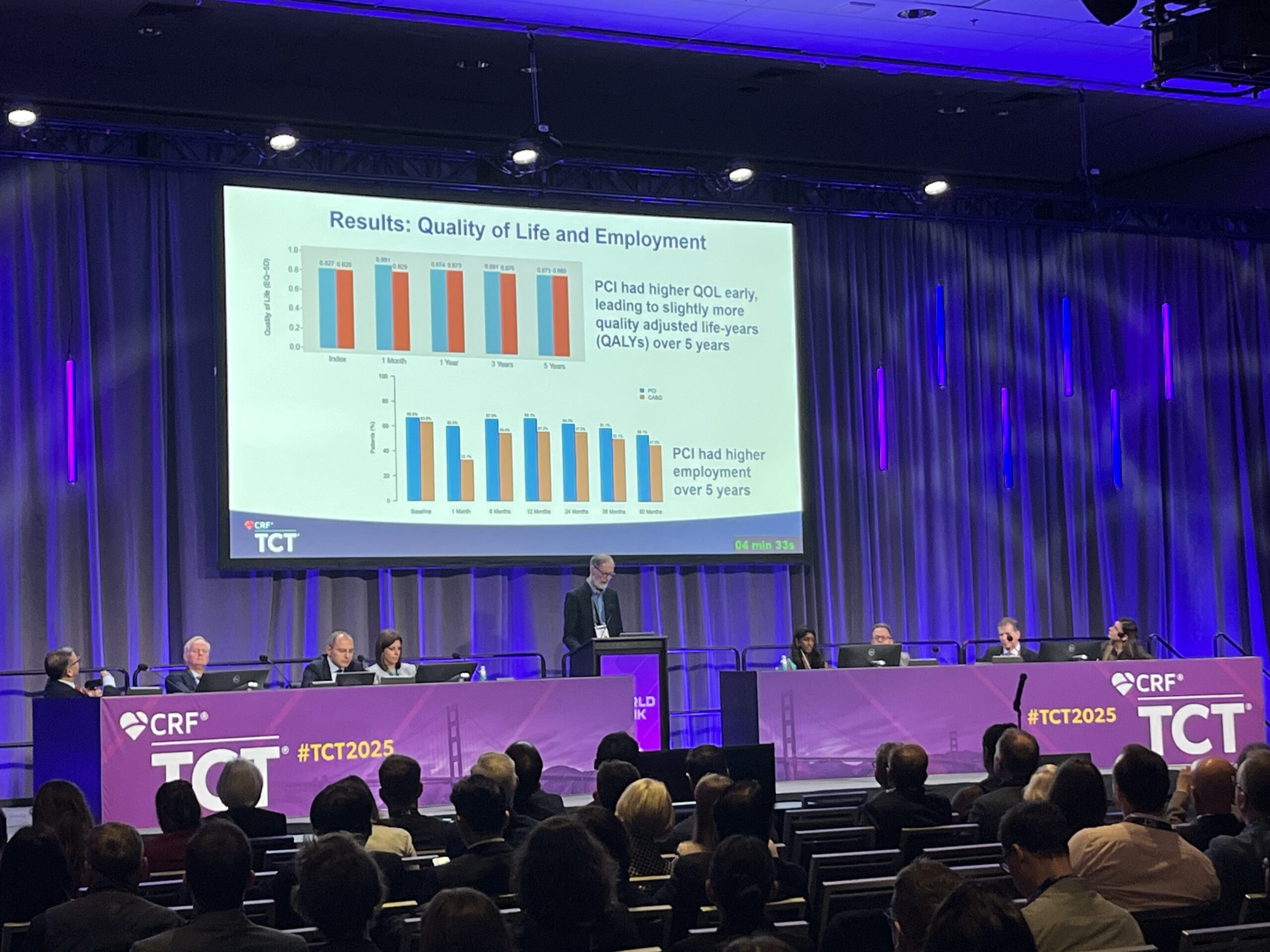
The investigators measured quality of life at regular intervals throughout the trial and calculated the quality-adjusted life years (QALYs) of survival in each group of patients, Hlatky detailed. They then performed an incremental cost-effectiveness analysis by looking at the difference in cost between CABG and PCI divided by the difference in QALYs between the procedures, using the benchmark of US$150,000 per QALY as the upper limit of willingness to pay.
“At one month, PCI patients had an edge in their quality of life, and subsequently, they were reasonably similar,” said Hlatky, detailing the results, adding that, over the five-year time period, there were more QALYs in the PCI patients. Cumulative QALYs of survival over five years of follow-up were numerically higher in PCI-assigned patients, although the difference was not statistically significant.
On the employment rate among patients who were 65 years or younger, Hlatky detailed that at one month, “PCI patients were largely back to work, while the CABG patients were not”.
The JACC paper details that by one year of follow-up, employment was above baseline levels among PCI-assigned patients but was lower than baseline in the CABG-assigned patients. Employment rates then declined over continued follow-up in both groups but were significantly higher among PCI-assigned patients at each time point. At five years, 56% of PCI-assigned patients were employed, compared with 47% of CABG-assigned patients
The cost of the index procedure was significantly higher in CABG-assigned patients, though the difference in cumulative costs between the groups narrowed over the five years of follow-up because of higher follow-up costs in the PCI group. However, cumulative costs were still significantly higher among CABG-assigned patients at five years (US$39,990 vs. US$25,667).
The cumulative cost over five years was 30% higher for CABG-assigned patients than for PCI-assigned patients and remained 22% higher in a sensitivity analysis that increased the cost of the index PCI by 10%.
In his concluding remarks, Hlatky said that the analysis had demonstrated lower costs for PCI than CABG, both over the five-year trial period and lifetime projections. “PCI led to more quality-adjusted life years of survival, both within the five years and the lifetime projections,” he said. “These results are different from those of the three previous trials that found CABG to be cost effective—and the reason is fairly simple—mortality did not differ between PCI and CABG in FAME-3, so there was no survival advantage among the CABG patients to offset its higher long-term costs.”
At TCT, Hlatky was asked how clinicians should extrapolate the findings, given that costs will differ greatly in different regions. Hlatky said it is important to separate cost and resource use when weighing up the study.
“The thing that’s different mostly between countries is the prices that we pay for things, not so much the resources,” he commented. “If you go to any country, more resources are required to do CABGs than they are to do PCI. And so certainly, we can look at this using alternative costing systems, but other studies have done this, and the results are similar in saying the relative prices matter more than the absolute prices.”