An analysis of the rates and clinical implications of alternative definitions of procedural myocardial infarction (PMI) used in the EXCEL trial has been published in the Journal of the American College of Cardiology (JACC). The analysis has led the EXCEL investigators to conclude that while relative rates of PMI after percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) vary according to definition, the protocol definition of PMI used in EXCEL is justified.
An analysis of the rates and clinical implications of alternative definitions of procedural myocardial infarction (PMI) used in the EXCEL trial has been published in the Journal of the American College of Cardiology (JACC). The analysis has led the EXCEL investigators to conclude that while relative rates of PMI after percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) vary according to definition, the protocol definition of PMI used in EXCEL is justified.
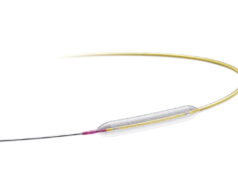
EXCEL was an international, open-label, multicentre, randomised trial that compared PCI using an everolimus-eluting stent (Xience, Abbott) and CABG for the composite endpoint of death, myocardial infarction (MI), and stroke in patients with left main disease. The five-year findings were presented at the Transcatheter Cardiovascular Therapeutics scientific symposium (TCT 2019; 25–29 September, San Francisco, USA) and published in the New England Journal of Medicine (NEJM), and concluded there was no significant difference between the procedures. However, since the presentation of the findings, the definition of MI used in EXCEL has been under the spotlight after it was claimed that the parameters for MI set out in the trial directly influenced the outcomes.
The latest analysis sought to determine the rates and clinical relevance of PMI observed during the trial using different definitions: the original study protocol definition of PMI, which required a large elevation of creatine kinase-MB (CK-MB), with identical threshold for both procedures; and the Third Universal Definition of MI (types 4a and 5), which required lesser biomarker elevations but with supporting evidence of myocardial ischemia, different after PCI and CABG.
In the analysis, John Gregson (London School of Hygiene and Tropical Medicine, London UK), Gregg W Stone (Icahn School of Medicine, Mount Sinai, New York, USA), and colleagues write that while the UDMI criteria for non-PMI have been widely adopted, achieving consensus on a single best definition for PMI has been more challenging, with different definitions for PMI having been used in the major trials of coronary revascularisation.

“The rates of PMI may vary greatly depending on the definition used, especially with high-sensitivity troponins that detect myonecrosis after the majority of revascularisation procedures. Thus, the optimal PMI definition remains undetermined, and the implications of this choice on the outcomes and interpretation of clinical trials have not been formally studied,” they write.
After analysing the EXCEL results using the two PMI definitions, the study team notes that the absolute rates of PMI after PCI and CABG did vary according to the definition, with PMI after PCI occurring in 3.6% of all protocol definition patients, compared to 3.3‒4.6% of patients by the Third UDMI. PMI after CABG occurred in 6.1% of all patients by the protocol definition, and in 1.4‒3.5% of patients by the Third UDMI.
“As a result, the relative rates of PMI after PCI versus CABG varied by definition,” the analysis finds. “PMI rates were lower after PCI compared with CABG by the protocol definition, were higher after PCI compared with CABG using the Third UDMI CK-MB or mixed biomarker definition, and were not significantly different after PCI and CABG using the Third UDMI troponin definition. In the intention-to-treat population (n=1,905), the rates of the primary endpoint of the EXCEL trial (the composite of death, all MI, or stroke) were similar after PCI and CABG at three and five years when using the pre-specified protocol definition of PMI, but were greater after PCI compared with CABG when PMI was determined by the Third UDMI.” Additionally, the analysis found that the protocol definition of PMI was associated with increased cardiovascular death, with a similar risk after both PCI and CABG.
Discussing the findings, the study team writes that the principal conclusion of any randomised trial “must of course rely on the pre-specified primary endpoint”.
“Nonetheless,” they add, “given the potential impact on clinical trial interpretation, a pressing concern is identifying which of the numerous definitions of PMI in widespread use is optimal for endpoint determination.
“In this regard a generally accepted principle is that each component of a composite primary endpoint should be of prognostic importance. In addition, the prognostic relevance of an endpoint should be similar with both treatments to afford a fair comparison.” The study team goes on to suggest that the protocol definition of PMI used in EXCEL met these criteria, as it was independently associated with subsequent cardiovascular and all-cause death during five-year follow-up, with similar hazard after PCI and CABG. In contrast, they add, PMI using the Third UDMI was “very strongly” associated with subsequent mortality after CABG but was not associated with mortality after PCI. “Accordingly, the originally established protocol definition of PMI provides a better basis for reliable comparisons,” they argue.