Analysis of one-year results from the NOTION-2 trial, in which investigators compared transcatheter aortic valve implantation (TAVI) to surgical aortic valve replacement (SAVR) in younger, low-risk patients, point towards less favourable outcomes after TAVI in patients with bicuspid aortic stenosis.
Key results of the trial were presented as late-breaking research by Ole De Backer (Rigshospitalet, Copenhagen, Denmark) at EuroPCR 2024 (14–17 May, Paris, France). De Backer described the trial as the first to randomise younger, low-risk patients with either tricuspid or bicuspid aortic stenosis to a transcatheter or surgical approach.
Though he cautioned that the findings warrant validation in larger randomised studies and that further follow-up out to five and eventually 10 years will shed further light on the initial results of the trial, De Backer commented that the findings may have implications for the treatment of younger patients with aortic stenosis and bicuspid valve anatomy.
The study, which took place in Northern Europe, randomised 370 patients aged 75 years or younger to compare the clinical outcomes obtained with TAVI versus surgery at 12 months.
“There are already current TAVI versus SAVR low risk trials, but in all of these trials typically older patients are included and bicuspid aortic valve stenosis has always been excluded,” De Backer told journalists at a press conference where he previewed the results of the trial.
Participants in NOTION-2 were between 60 and 75 years of age, with 187 randomised to the trial’s TAVI arm, and 183 to the surgery arm. In the TAVI arm, 72.7% of patients received a self-expanding device. Investigators studied a composite primary endpoint of death, stroke or rehospitalisation related to procedural, valve or heart failure.
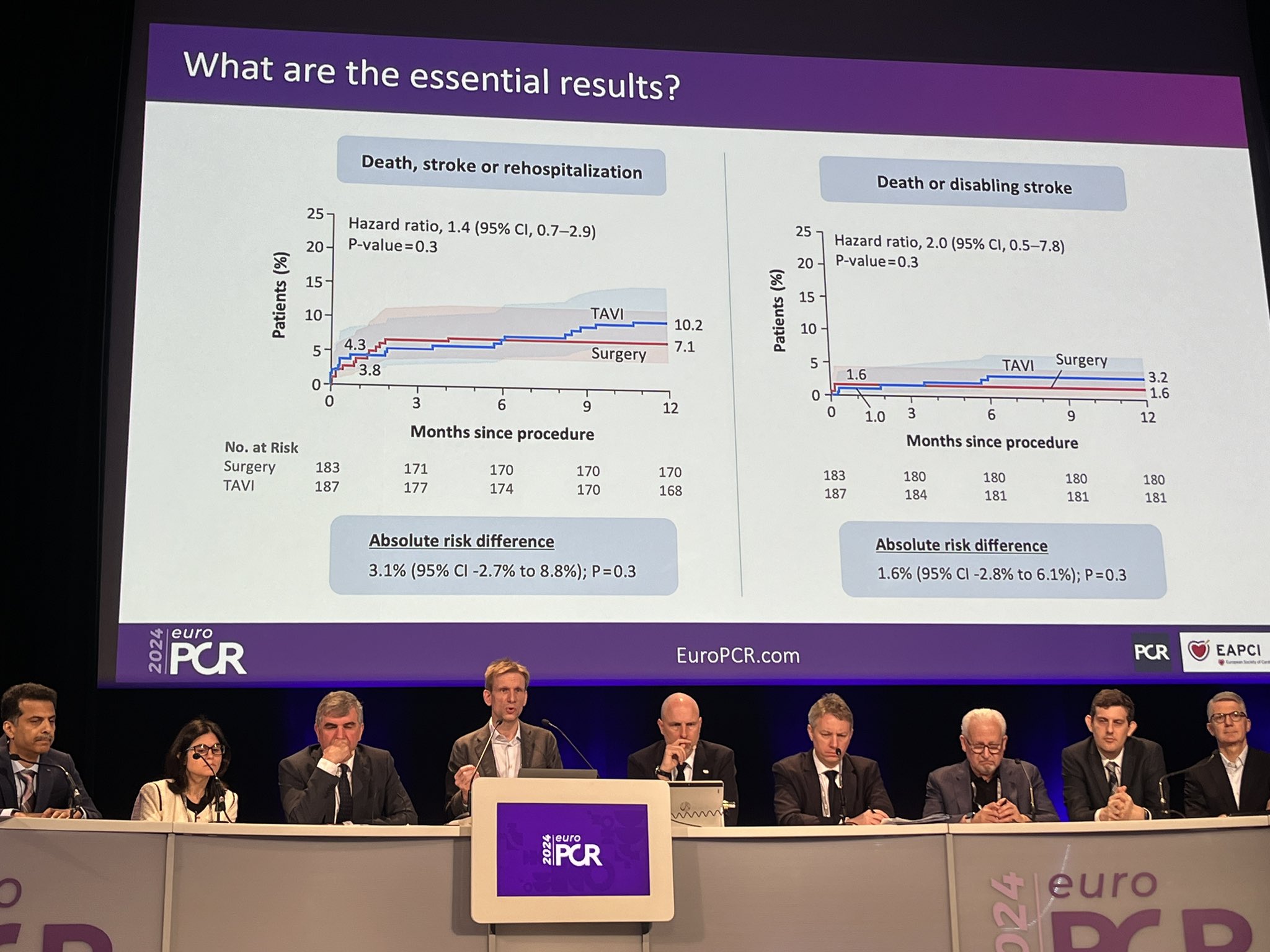
Death, stroke or rehospitalisation occurred in 10.2% of patients in the TAVI arm, versus 7.1% in the surgical arm, with an absolute risk difference of 3.1%, which fell below the trial’s prespecified non-inferiority margin of 5%, although De Backer noted the upper limit 95% confidence interval (CI) surpassed this prespecified margin.
On the incidence of the co-primary endpoint of death or disabling stroke, De Backer noted that this was extremely low in both arms, totalling 3.2% in the TAVI arm versus 1.6% in the surgical arm, resulting in an absolute risk difference of 1.6%.
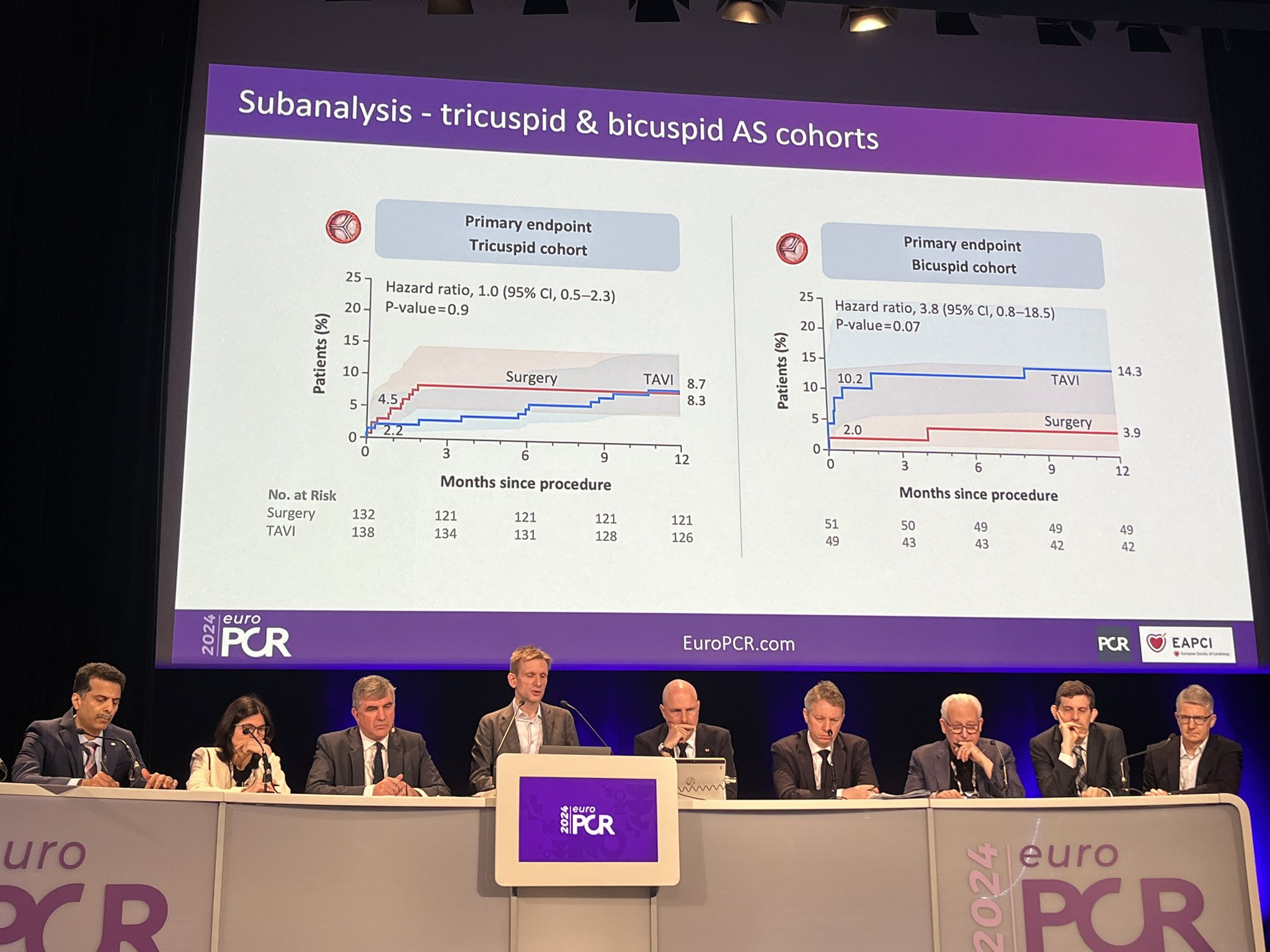
Significantly, De Backer reported that the investigators performed separate sub-analyses in the tricuspid patients, who made up 74% of the overall patient cohort, and the bicuspid patients, who represented closer to 26% of patients. De Backer said that though this was “largely underpowered, it gives us a nice indication of where these results go to”.
De Backer described the results in the analysis of tricuspid patients as showing clinical equipoise for TAVI versus surgery, with a percentage point risk difference of 0.4 between the two therapies for death, stroke or rehospitalisation. However, in bicuspid patients, the risk difference for this same measure stood at 10.4 percentage points favouring surgery, with the risk difference for stroke equating to 6.1 percentage points in favour of SAVR.
“We have to be modest of course—this is still a rather limited study population overall—but still we believe that this may impact future randomised controlled trial designs comparing both therapies, especially in this bicuspid cohort,” De Backer said, summing up his view of the findings. “Eventually, it may have impact on the guidelines, but this study is underpowered for that. For sure, it may impact what we may do if we have to treat younger, bicuspid patients with TAVI.”
De Backer elaborated further on this point when asked during the press conference what his recommendation would be at present for the choice of therapy in younger patients with a tricuspid or bicuspid valve.
“I want to repeat that we have to be humble about the data,” he said. “It should be an encouragement for further studies in this field in these really young patients. The signal we see is that, especially in tricuspid aortic stenosis patients, the clinical outcomes are equally good with TAVI or surgery; this is with a follow-up of one year. The choice for TAVI or surgery could, or should, depend more on the overall lifetime management options for these patients. Anyway, it could be time to consider both therapies in this patient population with an age of 60–75 years, as long as the patients have a tricuspid valve.”
For patients with bicuspid valve anatomy, De Backer commented that the NOTION-2 results point toward a need for clinicians to be more selective in which bicuspid patients to offer TAVI and to consider the use of cerebral embolic protection when proceeding with TAVI in young bicuspid patients.










