The European Society of Cardiology (ESC) has issued updated guidelines on the management of chronic coronary syndrome, with new recommendations covering diagnosis, timing of revascularisation, and a stronger emphasis on the use of intracoronary imaging to guide revascularisation procedures.
The European Society of Cardiology (ESC) has issued updated guidelines on the management of chronic coronary syndrome, with new recommendations covering diagnosis, timing of revascularisation, and a stronger emphasis on the use of intracoronary imaging to guide revascularisation procedures.
Released at ESC’s 2024 congress (30 August–2 September, London, UK), the guidelines should prompt cardiologists to rethink chronic coronary syndromes as caused “not only by blockages in large arteries but also by dysfunction of smaller vessels”, guideline committee co-chair Christiaan Vrints (Antwerp University Hospital, Antwerp Belgium) comments.
Speaking at a session to mark the launch of the new guidelines at the ESC meeting, Francisco Javier Rossello (Son Espases University Hospital, Palma de Mallorca, Spain), a member of the writing committee, detailed that the guidelines advocate a ‘stepwise’ approach to managing individuals with suspected chronic coronary syndrome, incorporating four pillars that encompass general assessment, further assessment, confirmation of diagnosis, and treatment.
Updates in the latest version include a focus on the diagnosis and management of angina/ischaemia with non-obstructive coronary arteries (ANOCA/INOCA) caused by coronary artery spasm or microcirculatory dysfunction. Recommendations state that persistently symptomatic patients with suspected ANOCA/INOCA who do not respond to guideline-derived medical therapy should undergo invasive coronary functional testing to determine underlying endotypes to guide appropriate medical therapy.
For individuals with symptoms suggestive of chronic coronary syndrome who have a low to moderate (>5%–50%) likelihood of obstructive coronary artery disease based on symptoms, age, sex and risk factors, the guidelines state that coronary computed tomography angiography (CCTA) is an effective means of ruling out coronary atherosclerosis or, at the other extreme, in estimating the risk of major adverse cardiovascular events based on disease anatomy.
Revascularisation
Indications for coronary revascularisation in the 2024 guidelines remain largely similar to the previous iteration of the document, published in 2018, namely: symptoms related to ischaemia that are refractory to medical therapy alone, and/or significant disease of the left main stem, of the proximal left anterior descending artery, or of multiple large epicardial arteries.
Selection of the revascularisation modality should be based on the patient’s profile, coronary anatomy, procedural factors, patient preferences, and outcome expectations, the guidelines state. Coronary artery bypass graft (CABG) surgery is favoured over percutaneous coronary intervention (PCI) in patients with diabetes or reduced left ventricular ejection fraction (LVEF, <35%), though PCI may be considered as an alternative to CABG in those who are non-operable or considered to be at high risk for surgery or with anticipated difficult rehabilitation.
Among patients with three-vessel disease without diabetes, CABG is recommended if the individual is not responding to medical therapy, but PCI is recommended in those with low-to-intermediate anatomic complexity.
Speaking at the ESC congress, Julinda Mehilli (Hospital Landshut-Achdorf, Landshut, Germany) stressed the importance of applying a shared decision-making process when considering these recommendations.
“We should apply a patient-centred decision, particularly for patients with LV dysfunction to choose between revascularisation or medical treatment,” said Mehilli, referring specifically to the recommendations relating to patients with reduced LVEF. “We need to have a careful evaluation, preferably by the heart team, of coronary anatomy, correlation between coronary anatomy and LV dysfunction, comorbidities, life expectancy, individual risk to benefit ratio, and what is the patient’s perspective.”
Intracoronary imaging
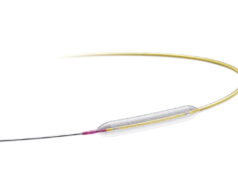
Among the major changes to the latest version of the guidelines is a new emphasis intravascular imaging. When performing revascularisation via PCI, intracoronary imaging—in the form of intravascular ultrasound (IVUS) or optical coherence tomography (OCT) —is deemed as being helpful to guide interventions and enhance results, especially in complex scenarios including left main disease, bifurcations, or long lesions.
“The change to a IA recommendation is based on a multitude of randomised controlled trials showing consistent substantial clinical benefit,” said Lorenz Räber (Bern University Hospital, Bern, Switzerland), highlighting the importance of this new recommendation to Cardiovascular News. “Europe is lacking behind, as many believe angio is enough, so the upgrade is expected to fuel the use of imaging for complex lesions. Currently, there is no other technical refinement of PCI that reportedly improves clinical outcomes to the degree observed with intracoronary imaging.”
“Meta-analysis of randomised clinical trials had already shown that intracoronary image guidance of PCI improves patient outcomes and saves lives,” said Javier Escaned (Hospital Clinico San Carlos, Madrid, Spain). “But the IA recommendation for IVUS in the updated ESC guidelines is crucial, as it reflects expert consensus based on a definite body of evidence supporting the positive impact of IVUS, specifically for patients with anatomically complex lesions treated with PCI.”
Intracoronary pressure measurement, fractional flow reserve (FFR), instantaneous wave-free ratio (iFR), or quantitative flow ratio (QFR) are recommended to guide lesion selection in patients with multivessel disease.
DCB or DES for in-stent restenosis?
Further recommendations apply when patients require a repeat revascularisation—representing around one in five of those undergoing CABG or PCI within five years, according to figures quoted within the guidelines. Significantly, recommendations favour the use of drug-eluting stents (DESs) over drug-coated balloons (DCBs) for the treatment of in-stent restenosis following PCI. This has elicited surprise from some corners, given that recent evidence has suggested that DCBs may be a favourable option in this scenario.
“I find it strange that after the positive results of the AGENT IDE trial, with consequently the possibility of using a DCB for in-stent restenosis in the USA (despite the lack of reimbursement so far), the ESC guidelines have decided to step back from a substantial equivalence in the indication in using a DCB or a DES, coming to favour a DES approach,” Bernardo Cortese (UH Harrington Heart & Vascular Institute, Cleveland, USA, and Fondazione RIC, Milan, Italy) tells Cardiovascular News.
Cortese points out that the recently published 10-year results of the ISAR DESIRE 3 trial—in which investigators compared PCI using paclitaxel-coated balloons and DESs for the treatment of in-stent restenosis— “showed substantial equivalence between DCB and DES from the clinical standpoint, with a signal of excess mortality in the DES group”, which, he says, makes it unclear why the guidelines now favour DES over DCB.
“I believe that we should run a modern study with an ad hoc protocol of lesion preparation before DCB or DES, with a stepwise implementation of intracoronary imaging during all the stages of ISR-PCI.”
Cortese also expressed surprise at the absence of an indication for DCB as a therapeutic alternative in the de novo setting, highlighting that several trials have shown good outcomes compared to stents, with similar or improved angiographic performance, along with improved long-term performance. A patient-level meta-analysis to be presented by Cortese at TCT 2024 (27–30 October, Washington, DC, USA)—ANDROMEDA—will offer yet further evidence in this area, he says.