A sub-analysis of the Recre8 trial, assessing patients at high bleeding risk (HBR) undergoing percutaneous coronary intervention (PCI) who received a short course of dual antiplatelet therapy (DAPT), saw a higher rate of clinically relevant bleeding in HBR patients during DAPT.
Findings of the analysis were presented as a pre-recorded abstract during the Cardiovascular Research Technologies meeting (CRT 21 Virtual, 13 February–24 April) by Nicole van Hemert (University Medical Center Utrecht, Utrecht, The Netherlands).
Recre8 was a multicentre trial, carried out in Northern European hospitals, comparing the clinical efficacy and safety of the polymer-free Cre8 (Alvimedica) amphilimus-eluting stent to the Resolute Integrity (Medtronic) permanent-polymer zotarolimus-eluting stent.
The all-comers PCI trial, included patients with ischaemic heart disease who required PCI involving implantation of a drug-eluting stent. There were no exclusion criteria based upon clinical presentation or lesion characteristics, van Hemert explained, although for instance patients with revascularisation prior to a transcatheter aortic valve implantation (TAVI) procedure were excluded.
Patients were stratified for their troponin status at baseline, to assess whether they had troponin-positive or troponin-negative disease, and whether they had a history of diabetes, and were randomised for implantation to either the Resolute Integrity or Cre8 stent.
Those with troponin negative disease included in the current analysis were treated with one month of DAPT, after which they continued with aspirin monotherapy.
The goal of the study was to establish noninferiority of the polymer-free stent compared to the polymer stent with an endpoint of target lesion failure, which was a composite of cardiac death, target vessel myocardial infarction and target lesion revascularisation.
Results after one year from the whole population have been previously published, in which non-inferiority of the polymer-free amphilimus-eluting stent was demonstrated, van Hemert detailed.
Offering an overview of the baseline and lesion characteristics in the current study population, van Hemert noted that 23% of patients had diabetes, 26% had already had a PCI, and 12% had previously undergone coronary artery bypass grafting (CABG). Regarding lesion characteristics, she explained that 55% had complex lesion anatomy and 40% of patients presented with multivessel disease at coronary angiography at inclusion.
High bleeding risk (HBR) was defined in line with the consensus document published by the Academic Research Consortium (ARC), as a risk of BARC 3 or 5 type bleeding of ≥4% or more after one year, or the risk of intracranial haemorrhage (ICH) of ≥1% at one year.
Van Hemert said: “In the consensus document, the ARC proposes criteria for high bleeding risk, in which patients with one major or two minor criteria are classified as being high bleeding risk. This is important because patients with high bleeding risk are often excluded from clinical trials, and if they are included the definitions used for high bleeding risk differ greatly and consensus-based definitions can improve the interpretation and generalisability of these clinical trials, as has been proven to be true with the broadly used endpoint definitions by the ARC.”
A total of 892 patients from the Recre8 trial determined to be troponin negative received one month of DAPT, of which 193 (21.6%) were identified as being high bleeding risk.
The primary endpoint of target lesion failure was found to be similar between the non-high bleeding risk and high bleeding risk groups (6.4% vs 8.3%, p=0.37), van Hemert said, but commented that when looking at the broader endpoint of net adverse clinical events (NACE), a composite of all-cause death, myocardial infarction, unplanned revascularisation, stroke and major bleeding, this was almost twice as high in the high bleeding risk group (11.2% vs 20.7%, p=<0.001).
She added: “When we look at the ischaemic NACE, removing major bleeding from this composite endpoint, we see that this is still significantly higher in the high bleeding risk group, and this shows that this population is not only at risk for bleeding events, but also for ischaemic events.”
Looking at the bleeding endpoints including BARC 3 or higher bleeding, this was found to be twice as high in the high bleeding risk group (1.3% vs 2.6%, p=0.19), although not a significant difference, van Hemert said.
“As a lot of events occur in the first 30 days, when the patients are on dual antiplatelet therapy, we have also performed a landmark analysis disregarding these first events. During aspirin monotherapy we see that the numerical difference between bleeding risk and not high bleeding risk is smaller, however, as it was already not significant between 0–12 months, this is also not a significant difference,” she added.
This was also done for BARC 2 or higher bleedings, disregarding the first 30 days. “We still see a rate that is three times as high in the high bleeding group, however the difference is not significant any more,” van Hemert detailed.
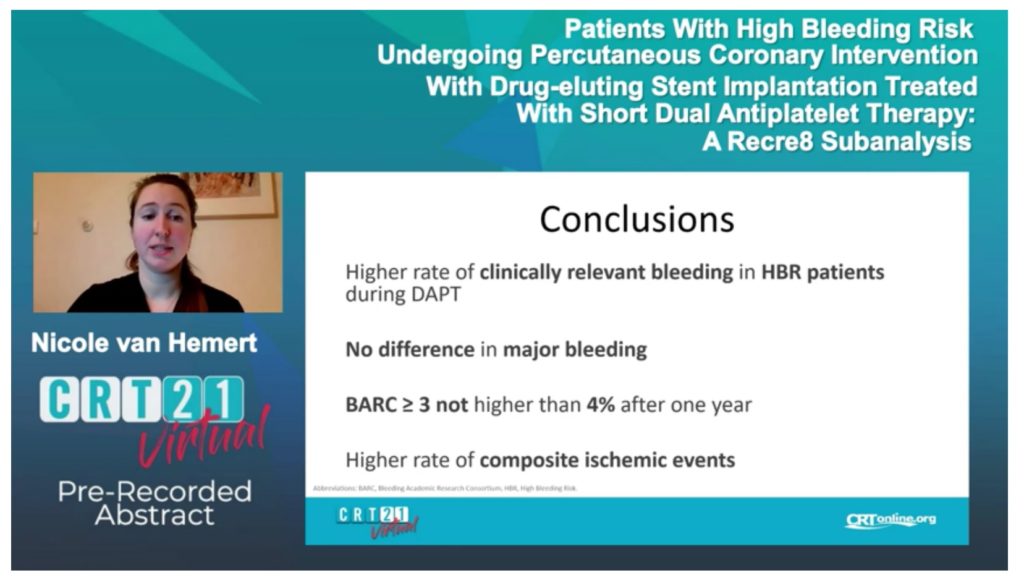
In her conclusion, she noted that a higher rate of clinically relevant bleeding in high bleeding risk patients was observed during dual antiplatelet therapy, and the rate of clinically relevant bleeding remains three times as high during aspirin monotherapy.
“We see no statistically significant difference in major bleeding between the non-high bleeding risk and bleeding risk groups, suggesting that in this case, these patients are not doing much worse during aspirin monotherapy as compared to the non-high bleeding risk patients regarding major bleeding.
“We, however, do see that the rate of BARC 3 or higher is not higher than 4% after one year, which was the definition given by the ARC, so there is a possibility that because some of the variables were missing in our dataset, patients were wrongly classified as not being high bleeding risk, even though they should have been classified as high bleeding risk.”
Ending her presentation, she noted that the study team also observed a higher rate of ischaemic events, “Showing that these patients are not only at risk for bleeding, but also for ischaemic events, making it all the more important to establish a suitable treatment strategy for these patients”.










