Coronary artery bypass graft (CABG) surgery is associated with significantly lower all-cause and cardiovascular mortality risk and longer median survival time compared to percutaneous coronary intervention (PCI) in patients with diabetes and multivessel coronary artery disease, a new analysis from the SWEDEHEART registry has shown.
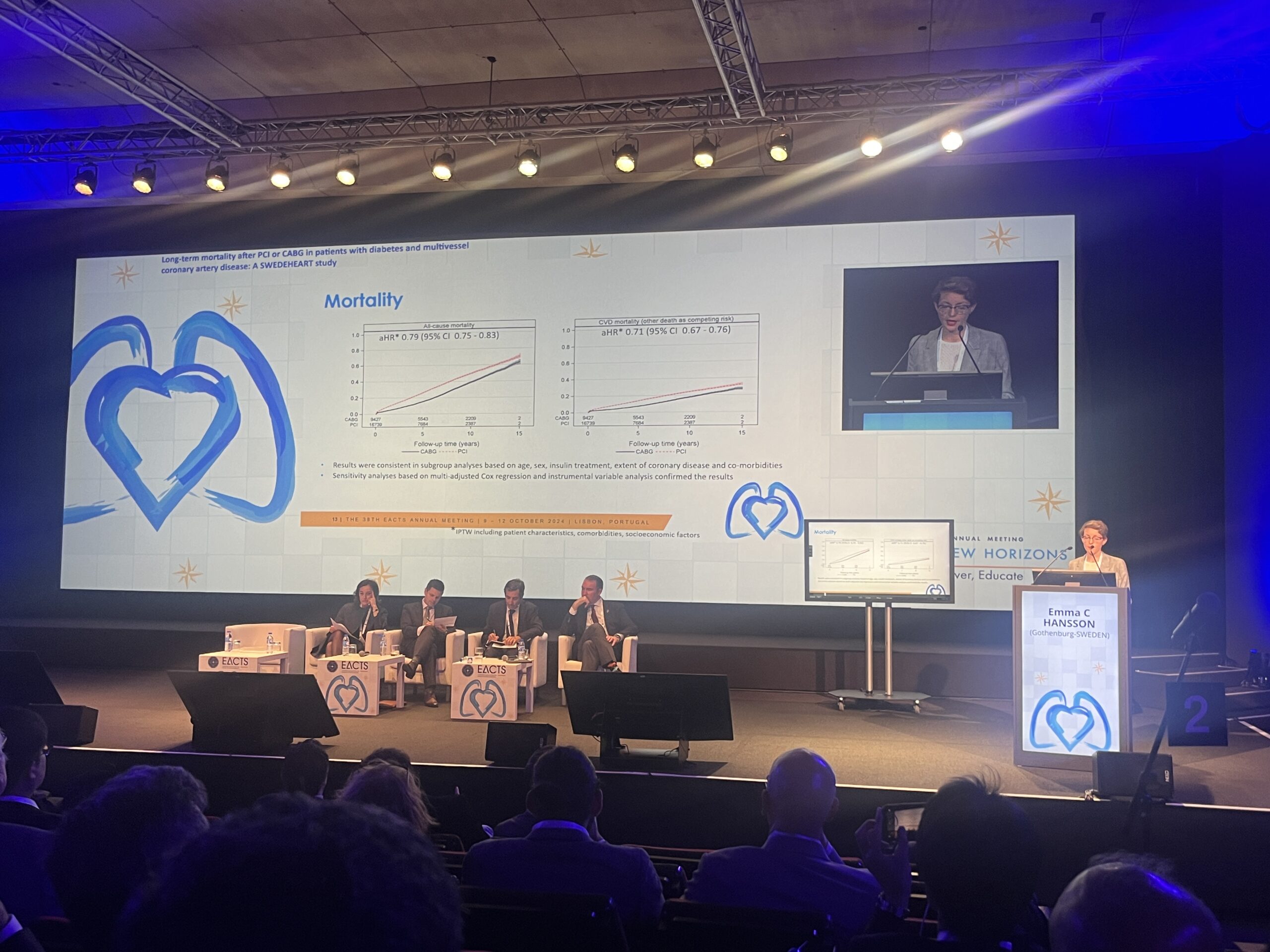
These findings were presented by Emma Hansson (University of Gothenburg, Gothenburg, Sweden) as late-breaking science at the European Association of Cardio-Thoracic Surgery (EACTS) 2024 annual meeting (9–12 October, Lisbon, Portugal).
SWEDEHEART is the Swedish national registry recording the outcomes of patients hospitalised for acute coronary syndrome or undergoing coronary or valvular intervention within the country.
Hansson and colleagues used data from the registry, alongside the country’s coronary angiography and angioplasty registry and other healthcare registries, with information on hospitalisation, drug prescription, socioeconomic status and mortality, to quantify and calculate the mean survival time after CABG or PCI, as well as looking at differences in various sub-populations.
Data were gathered for all revascularisations taking place between 2006–2020, excluding emergency cases, giving a total of 26,166 patients with multivessel disease and diabetes. Of these, 64% underwent PCI and 36% underwent CABG, with data available at a median follow-up of five years.
Hansson noted that there were important differences in the groups at baseline, with CABG patients having more left main stenosis, three-vessel disease, and previous myocardial infarction (MI), whereas PCI patients were typically older, more had heart failure and more had atrial fibrillation (AF).
The investigators noted that there were differences in which treatment patients were likely to be offered based upon where in the country they lived, with patients in some regions eight times more likely to have PCI than in others.
CABG was associated with a lower rate of all-cause mortality, Hansson detailed, with cardiovascular mortality also lower among patients who underwent surgery. Surgical patients had a median survival benefit that was 0.9 years greater than those undergoing PCI, she noted, with this benefit seen to be larger among women (1.5 years).
Hansson also reported a longer survival time in patients with left main stem stenosis, who gained a median of 4.3 years if they underwent CABG versus PCI. In patients with three-vessel disease, there was also a “pronounced” increase in median survival, she noted, though in those with a lower complexity of disease the same effect was not observed.











